Patellofemoral pain syndrome, or PFPS, describes pain in the front of the knee after sitting with your knees bent for a while, especially when you sit in a tight space on a long flight or in a movie theater. Sometimes PFPS is called “runners’ knee”, which is a vague term to describe PFPS in runners.
Women are twice as likely to get PFPS than men, according to a U.S. military study of more than 1,500 people as well as a review about female athletes and PFPS.
Causes
Overuse or overload are two common risk factors that cause PFPS. These factors can be increased by too much running, too much load over a long period of time, or even a lack of movement like sitting all day. While there’s no single cause of PFPS, researchers have found several factors why women are more likely to get PFPS.
Increased Q-angle
Women generally have wider pelvises, which increases the Q-angle (the angle between the quadriceps muscle and the patellar tendon). A larger Q-angle can lead to increased lateral forces on the patella, predisposing women to patellar tracking issues and PFPS.
Quadriceps muscle weakness
Weak muscles in the legs may cause PFPS. Some muscle problems that can lead to PFPS are weak knee muscles, uneven strength in parts of the quadriceps, and weak hip muscles. Weak quadriceps are linked to PFPS.
However, one study found no difference in hip muscle strength between female runners with and without PFPS. Some newer studies suggest that female athletes with stronger hip muscles might be more likely to get PFPS.
Increased knee valgus
Women often exhibit increased knee valgus, or “knock knee” alignment, which can increase lateral patellar tracking and stress on the patellofemoral joint.
Hormonal factors
Fluctuations in hormones, such as estrogen and relaxin, during the menstrual cycle may contribute to increased laxed ligaments and knee instability in women, increasing the risk of PFPS.
Anatomical variations
Women may have anatomical variations in the shape and size of the patella, trochlear groove, or femoral condyles, which can affect patellar tracking and increase the risk of PFPS. But keep in mind that the association between patellar tracking and knee pain is weak.
Increased hip internal rotation
Studies have shown that women tend to exhibit increased hip internal rotation during activities like running and jumping, which can alter patellar tracking and contribute to PFPS.
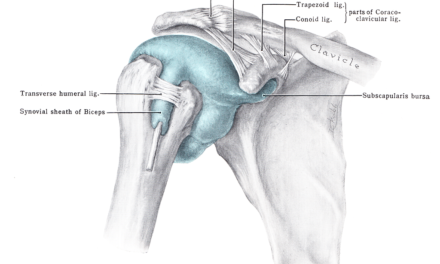
Anatomy of the knee
The kneecap or patella is a large, triangular-shaped bone that can be felt on the front of the knee joint. It articulates with the trochlear groove of the femur, and sits there loosely when you straighten your knee. A vertical ridge on the back of the patella divides it into the lateral and medial facets, along with the odd facet on the most medial part of the kneecap, that touches femur during full knee flexion.
During full knee extension, only the lower part of the patella is in contact with the femur. The patella is rather unstable in this position, and so, it’s more likely to dislocate at this angle.
Besides these up and down movements, the patella can tilt sideways in both directions (inside and outside) and rotates slightly inward and outward. So, the motion of the patella is more complex than what we can see on the surface.
The quadriceps muscle, which extends the knee, inserts onto the patella with the help of the quadriceps tendon. It surrounds the patella as the patellar tendon, which then inserts from the inferior border of the patella to the tibial tuberosity.
The knee ligaments help stabilize and move the joint include:
- anterior cruciate ligament (ACL)
- posterior cruciate ligament (PCL)
- medial collateral ligament (MCL)
- lateral collateral ligament (LCL)
- arcuate ligament
- posterior oblique ligament
- oblique popliteal ligament
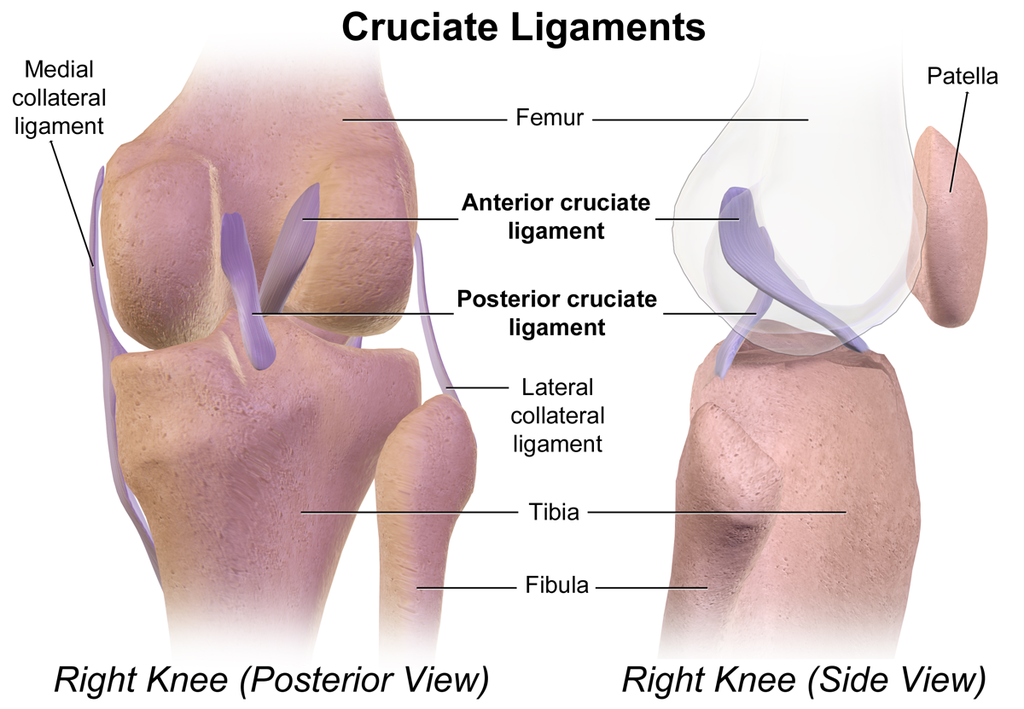
Image: BruceBlaus
When discussing the biomechanics of the knee joint, it’s important to describe the quadriceps force vector, which is the direction in which the patella will move upwards when you straighten your knee since there are many muscle fibers that pull on it from different directions.
This means that the inwards force keeps the outward force in check, preventing the kneecap from sliding out during a forceful knee extension movement, thus preventing knee dislocation.
The combined coordination of the nerves, tendons, muscles, and ligaments provide stability to a “floating” patella. But this is also one of the primary processes that leads to PFPS.
Diagnosis of PFPS
The most common symptoms of PFPS are anterior knee pain that often gets worse with squatting, stair climbing, and too much sitting. All these activities cause repeated stress on the knee joint as they load the joint in a flexed position for a long period of time.
Clinical findings may also include a positive patellar tilt test. Differential diagnosis of PFPS is based on the patients’ complaints with specific movements mentioned above, along with a positive patellar tilt test. It’s where a physician or physical therapist compares two or more conditions that may cause your symptoms since many types of knee pain share the same features, such as medial meniscus tear and IT band syndrome.
If you see a healthcare provider for anterior knee pain, they may rule out some other causes of this pain before diagnosing the condition as PFPS. The classification of PFPS is based on broad categories of findings that may lead to anterior knee pain
The American Physical Therapy Association (APTA) has published clinical practice guidelines (CPG) to classify PFPS based on the findings of the clinical exam to make treatment easy and more efficient. This is known as the impairment-based treatment protocol.
Basically, the classification system guides clinicians to the best course of action based on whether the knee pain exists with the overuse or overload without other issues like movement coordination impairment, reduced knee strength, and reduced knee flexibility. Each category is defined by the impairments noted that are the chief contributing factors to PFPS.
Finally, psychological factors such as fear avoidance, kinesophobia, pain catastrophizing, anxiety, and depression play a role in individuals with PFPS, just as they do with any other musculoskeletal pain.
If you happen to visit a physician or a physical therapist for anterior knee pain, they will rely on the clinical history as their primary “pain symptom checker” along with the examination findings discussed previously as their primary method of diagnosis of PFPS.
Treatment
Patients with PFPS related to overuse or overload can benefit from patient education to understand activity pacing and modification techniques. Those who have PFPS because of poor movement coordination will benefit from gait retraining, which involves adjusting their running mechanics with changes in the foot strike combined with hip and knee exercises to re-train proper movement.
Exercise
Strength programs that focus on both the hip and knee have been found to improve symptoms of PFPS than hip or knee strengthening alone, according to a 2018 systematic review and meta-analysis that pooled data from 14 trials with 673 patients.
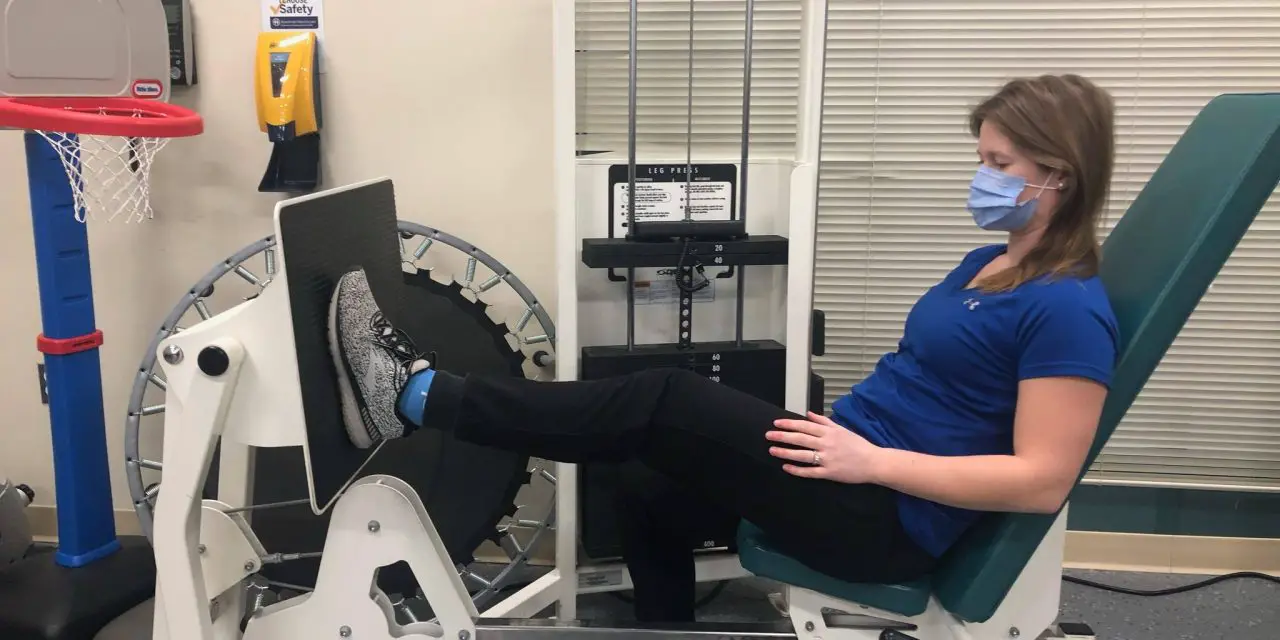
Exercises include open chain or close chain. An open-chain leg exercise is when your foot is free to move and your body is fixed in place. Sample open-chain exercises include leg extension, leg curl, and leg press.
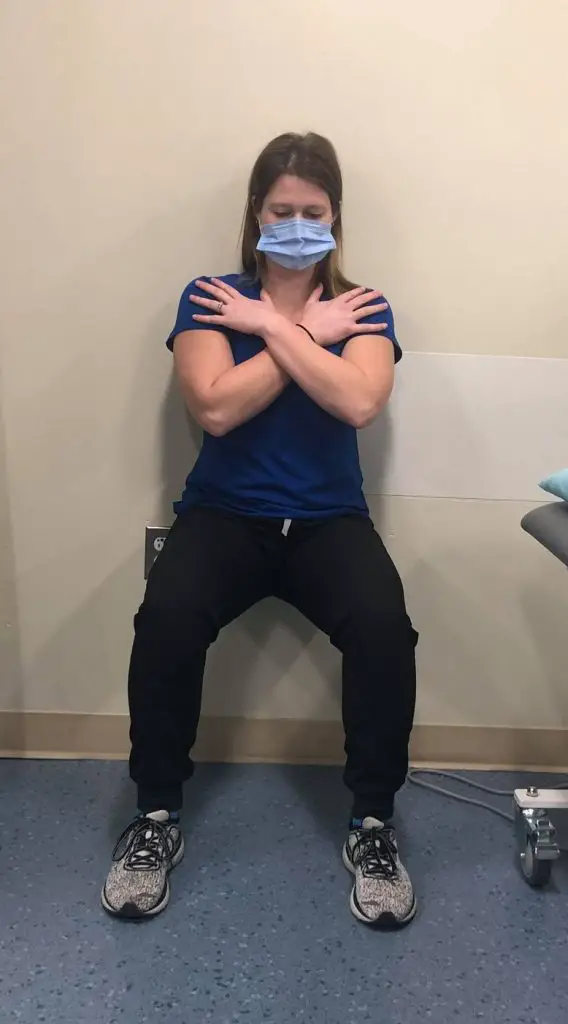
A closed-chain leg exercise is when your foot is fixed on the ground or another surface and doesn’t move. Examples would be a squat, lunge, and step-up. Both types of exercises have been shown to be almost equally effective whether they focus on the knee or hip.
A 2023 systematic review found that providing feedback to patients with PFPS can help reduce lateral movements of the knee when doing closed-chain exercises. Using braces alone didn’t affect knee movements, and taping didn’t change knee, hip, or ankle movements much.
A 2023 study of 200 patients with PFPS found that strengthening the quadriceps is just as good as strengthening the hips for reducing pain and improving function.
Stretching
Stretching may alleviate some knee pain and improve muscle flexibility, but it depends on what kind of stretching you’re doing. A 2021 study of 46 patients with PFPS found that dynamic stretching is better than static stretching for better muscle activation and reducing knee pain. However, there were not many differences in hamstring flexibility and knee strength between both groups. Not much is known whether dynamically stretching other muscles, such as the quadriceps or glutes, can elicit similar effects.
So instead of reaching for your toes to stretch your hamstrings, do leg swings front to back or side to side.
Related: How to Become More Flexible with Strength Training
Taping
Taping in athletics and manual therapy involves applying adhesive tape to the body to provide support, reduce pain, and prevent or treat injuries.
A 2023 review examined 50 research papers with nearly 1,500 participants. These studies focused on how Kinesio Tape affects pain, function/performance, strength, balance, and injury prevention. Overall, taping was mainly effective for reducing pain and not much else.
One 2021 systematic review found that Kinesio taping alone can help reduce knee pain up to four weeks for most subjects, but the effects wear off after six weeks. Also, there’s not much difference in pain at six weeks between those who used exercise only or Kinesio Tape with exercise.
One 2023 study of 20 patients with PFPS found that adding Kinesio Tape to exercise therapy “did not elicit extra benefit” quadriceps muscle strength and acceleration time and knee pain.
Also, research finds no difference in pain outcomes among Kinesio Taping, McConnell taping, and sham taping. In other words, all types of taping techniques can help reduce pain.
Related: Full review of taping for knee pain
While this article discusses the classification and treatment of PFPS, consult a healthcare professional for knee pain to rule out referral pain from other joints or other pathologies that may masquerade as PFPS.
Patellofemoral pain syndrome exercises
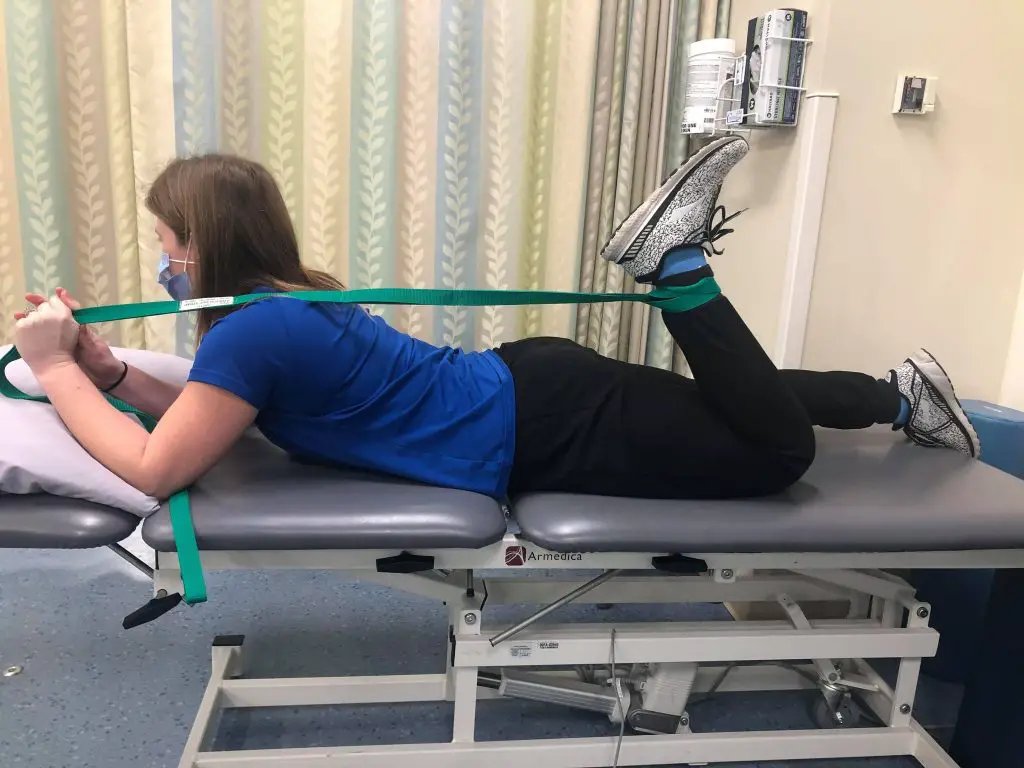
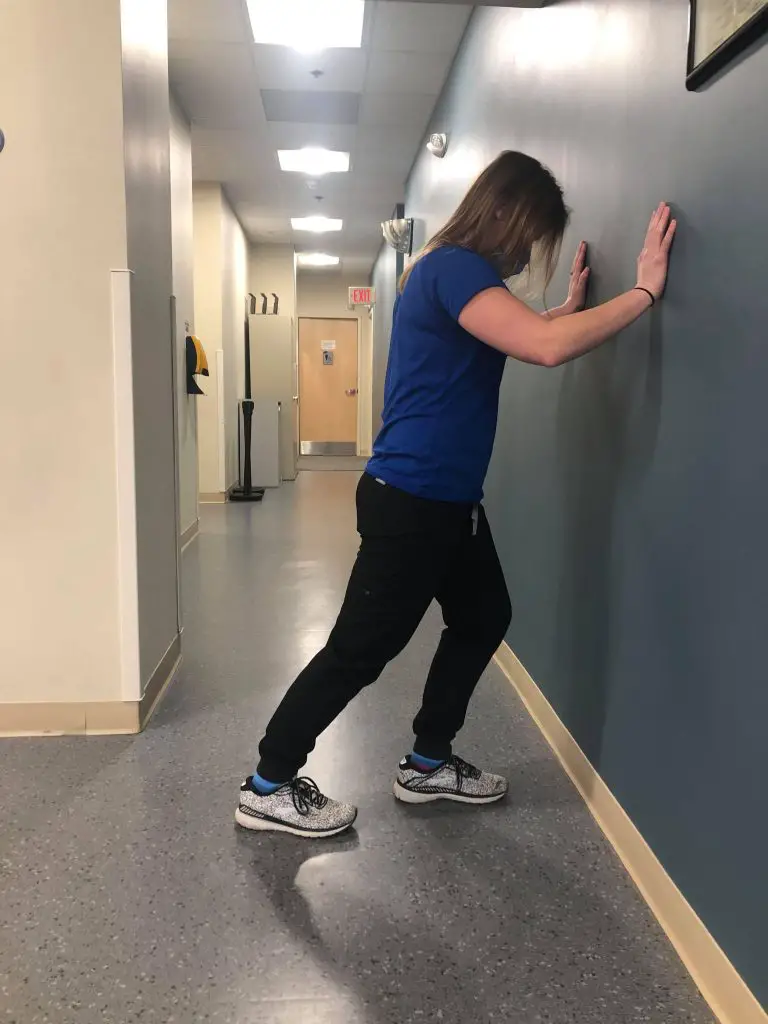
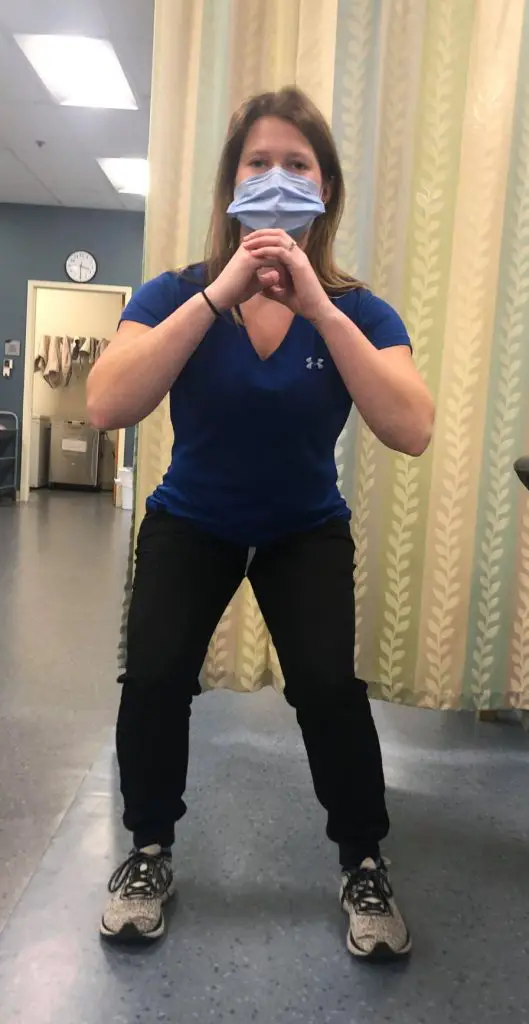
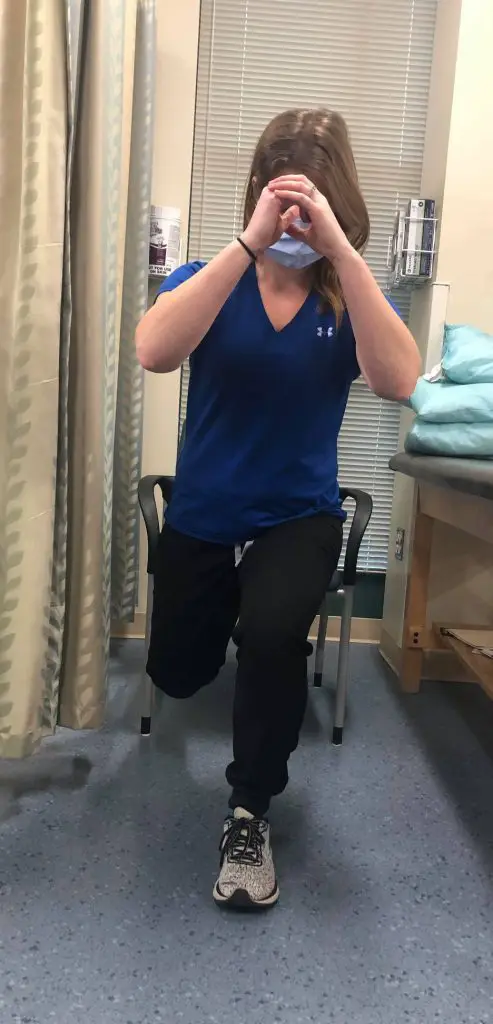
Your physical therapist may recommend a combination of open-chain and closed-chain exercises in your exercise program, which will likely chain and progress during your recovery. (All photos by Tanvi Maharaja)
Supine hip flexor stretch with band assistance
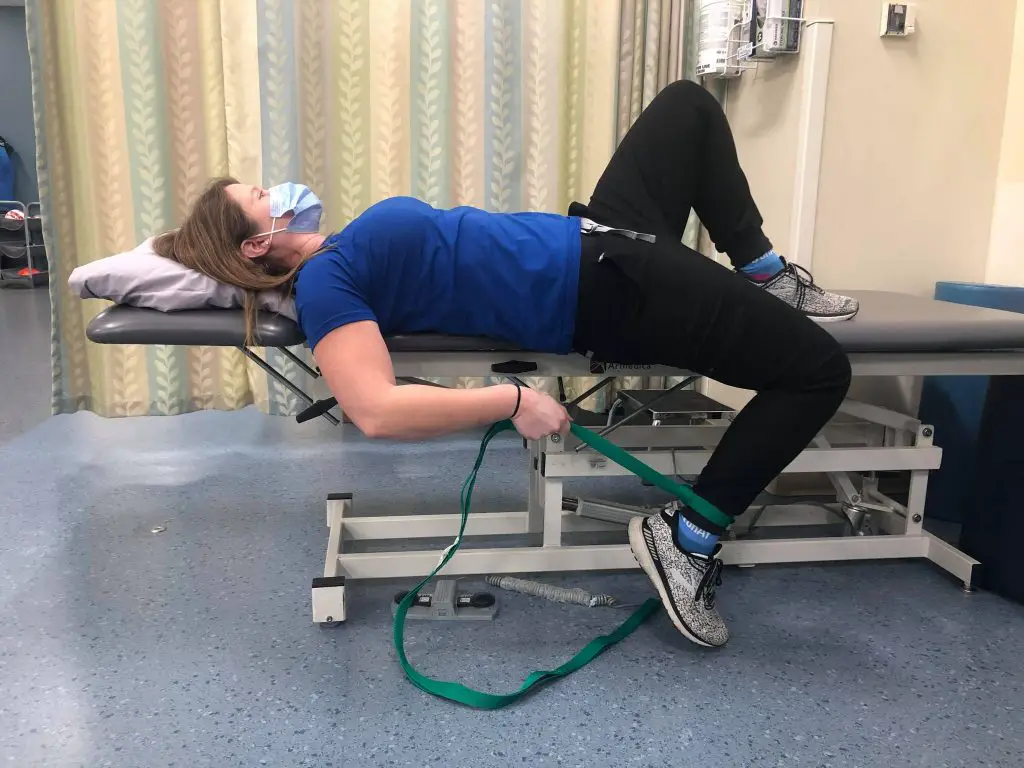
Prone quadriceps stretch with band assistance
Standing calf stretch
Single-leg balance

Squats
Leg press

Single-leg squat
Wall squats
Hip exercises include lateral walk with resistance band at knees. This can be progressed by having the band at the ankles and then to the forefeet.
Lateral walk with band

There’s a wide range of exercises for each category and exercises should be tailored to the individual’s needs and goals. Graded exercises along with optimal loading should be the goal with each exercise.
Pain management can be as simple as changing of your knee position often, or maybe performing some standing marches or taking a short stroll to minimize pain symptoms. Besides the biological and structural causes mentioned here, psychosocial perspectives should not be discounted.
When treating anyone, the patient’s psychosocial status matters just as much as the structural impairment. A holistic approach respecting the person as a whole, with their own beliefs, perspectives, and attitudes, shaped by past experience and encounters, will go a long way in better outcomes rather than zooming in on the knee.
Further reading
Why Does Bending Your Knee Hurts and What You Can Do

Tanvi Maharaja, DPT, OCS
My name is Tanvi Maharaja. I work as a Physical Therapist in an outpatient hospital setting in the Greater Boston Region. I have a Doctor of Physical Therapy degree, and I am a Board-Certified Specialist in Orthopedic Physical Therapy. I am also an eclectic practitioner of manual therapy, being a Certified Manual Therapist through NAIOMT, with a special interest in the spine. I love to write, cook, swim, and go on long walks to nowhere with my family.