A Bankart lesion is the most common type of shoulder dislocation where the humeral head of the upper arm bone moves toward the front and downward with applied force. This can cause the glenoid labrum of the shoulder socket to tear, making the shoulder joint less stable and more prone to repeat dislocations. Bankart lesions are common in athletes who participate in overhead sports but may also occur from a fall, car accident, or other stress to the shoulder.
There are two types of Bankart lesions:
Soft Bankart lesion: Only the labrum is torn without any associated bone damage. This is the most common type.
Bony Bankart lesion: Part of the glenoid bone is also fractured or broken off along with the labral tear. This can lead to significant bone loss and chronic instability.
A 2023 study of 790 cases of bony Bankart fractures in Sweden found that the average age was 57 years.
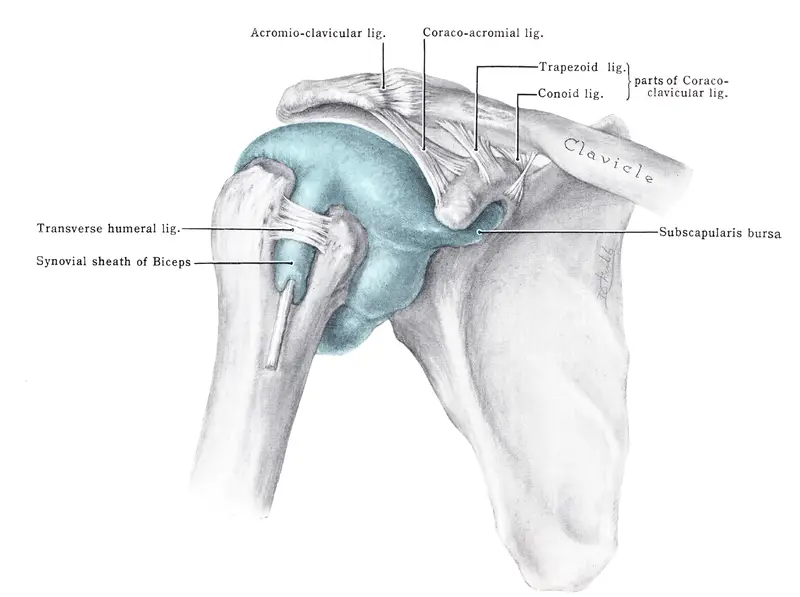
Anatomy of the glenohumeral joint
The shoulder joint is made up of the humerus, scapula and clavicle. The glenohumeral joint is formed by the head of the humerus and the glenoid fossa of the scapula. This joint is supported primarily by the glenohumeral ligaments (superior, middle, and inferior) and the muscles of the rotator cuff.
The inferior glenohumeral ligament is most often injured during a shoulder dislocation, resulting in a Bankart lesion.
The axillary nerve encircles the surgical neck of the humerus and may also be injured during shoulder dislocation or reduction. Axillary nerve injury will affect the deltoid muscle group and sensation to the proximal third of the upper arm.
Bankart lesion causes
Shoulder instability is often broken down into “born loose” or “torn loose.” Those who are born loose often have lax ligaments. These are often referred to as “double-jointed” because of their excessive range of motion. Those who injure their shoulder during a traumatic shoulder dislocation are torn loose.
Dislocation of the shoulder is a very common injury due to the lack of bony stability in the joint. It’s common in contact and collision sports and sports that have a high risk of falls, such as skiing or gymnastics. Bankart lesions may also occur during motor vehicle accidents or non-sports-related falls.
Those who participate in such sports or have a history of recurrent dislocations are more likely to suffer from a labral injury. Because many men in their teens and twenties participate in contact or collision sports, this group tends to see higher rates of Bankart lesion.
After a shoulder dislocation, clinicians must be cautious in preventing a Hill-Sachs lesion from developing. A Hill-Sachs lesion is a type of injury where part of the upper arm bone becomes compressed or indented due to the dislocation.
This change in the shape of the humerus can make the shoulder joint more unstable and prone to dislocating again, even with minimal force.
Symptoms
Common symptoms of a Bankart lesion is a sense of instability in the shoulder joint. If the injury is not immediately surgically repaired, patients sometimes have recurrent dislocations of increasing frequency and with less trauma with future injuries. In fact, recurrence rates in patients with first-time dislocations that are managed conservatively have been reported as high as 100%.
Clinically, these patients tend to have general shoulder pain that worsens with moving their arm into a typical throwing position or behind their back as if to reach a back pocket. These patients may be unwilling to move into certain ranges of motion because of fear that their shoulder will dislocate again.
Completing a course of care that uses the biopsychosocial model of pain (based on the neuromatrix theory) allows the patient to create a healthy habit that addresses previous experiences, values, emotions, and other factors that may influence their pain. Failure to address these components may lead to chronic pain.
Diagnosis
The gold standard for diagnosing a Bankart lesion is magnetic resonance arthrogram (MRA), but this does not mean the diagnosis can not be made in the clinic. Researchers in a 2016 study evaluated more than a decade of patient records to determine a cluster of tests that is clinically useful for diagnosing Bankart lesions. They found that a detailed patient history with positive findings on the anterior apprehension test and load and shift tests can diagnose anterior shoulder instability as consistently as imaging.
Anterior instability doesn’t always mean a Bankart lesion is present, but a history of repeated dislocations along with instability should make the clinician suspicious of a labral tear.
Patients who have non-traumatic Bankart lesions may not get to a clear cut diagnosis quickly. General shoulder pain when raising the arm is a common symptom that shouldn’t be taken for granted.
Shoulder impingement and bursitis can be ruled out with resistive testing where the finding is strong and pain free. Special tests for impingement may also be used to test the health of the shoulder. Without a reported dislocation, clinicians need to consider the patient’s story about their pain experience.
Treatment
Treatment for Bankart lesions depends on several factors, patient’s age, activity level, health history, and involvement in contact sports. These factors influence the risk of recurrent shoulder instability and guide the decision between surgical or conservative management.
Surgery
Surgical repair of Bankart lesions can be performed using an open or arthroscopic approach. The open approach has the best outcomes but it’s quite invasive and thus, rarely performed. The less invasive arthroscopic option allows the patient to build strength and return to their prior level of activity more quickly.
Arthroscopic repair of anterior labral tears involves placing suture anchors along the length of the tear to secure the tissue. The number of anchors is dependent on the size of the tear. Unlike SLAP tears where surgical repair of the labrum may or may not be warranted, immediate surgical repair is the treatment of choice for Bankart tears.
The failure and revision rates are significantly reduced when compared to conservative management of this injury. Arthroscopic repair is associated with an increased likelihood of a return to sports. Rehabilitation after surgery generally lasts six months or more, depending on the sport or activity the patient is returning to.
Conservative management
Conservative management of Bankart lesions usually begins with a period of shoulder immobilization followed by interventions to restore range of motion, improve strength, and enhance proprioception. Dislocating the shoulder is a traumatic experience that can create a fear of pain or movement.
To process pain and injury, patients who have a history of instability or are chronic dislocators should complete a course of rehabilitation that emphasizes restoring full range of motion, dynamic stability, and co-contraction of the muscles that support the glenohumeral joint. Failure to start a series of range of motion exercises in the appropriate time frame could lead to an even more painful condition, frozen shoulder.
A 2017 study suggests that a robust rehab program can restore strength in the injured arm in as few as six weeks. In their study, 12 first-time dislocators began the program two weeks after the injury. The program consisted of dozens of exercises, performed five times per week, using elastic bands and weights.
Although surgery is preferable, this program may be an option for bridging the gap between injury and a competitive sports season when there isn’t enough time to complete surgical intervention and rehab.
As with any injury or illness, consult with a physician or qualified medical professional to determine the best course of treatment.
History of Bankart lesion
Dr. Arthur Bankart first described the lesion in the British Medical Journal in 1923. Although glenohumeral joint instability was well recognized at the time, he didn’t think the surgical techniques being used were effective at restoring shoulder stability but rather overtightened the joint capsule which limited abduction.
Bankart showed his contemporaries that the shoulder capsule isn’t a naturally tense structure; rather that stability was lost from the detachment of the labrum from the glenoid rim. His repair was the first introduction to the use of sutures to repair the capsulolabral tissue.
Bankart lesion and massage therapy
Massage therapists working with patients who have Bankart lesions should obtain a detailed history. If the dislocation is recent, it’s important that patient positioning respects the vulnerable positions of the joint to minimize the risk of another dislocation.
Do not place their shoulder in abduction with external rotation or extension with internal rotation due to the laxity in the anteroinferior capsule. They will be more comfortable if their affected arm is supported by towels and pillows when supine so that the humerus does not drop below the midline of their body.
Those who have had a recent dislocation or who have chronic instability will have associated tightness in the muscles that support the shoulder. They may feel pain or tension in their upper trapezius and lateral cervical paraspinal muscles on the involved side from hiking their shoulder to raise their arm to avoid pain.
The posterior muscles of the shoulder have also undergone trauma during dislocation and may be stiff and tender following injury. Positioning the patient in a prone position with their arm supported on the table may be the easiest approach to target the posterior musculature. If this position isn’t well-tolerated, the patient may need to lie with their arm over the side of the table supported by an armrest.
Using the biopsychosocial model of pain control is likely the best approach to treatment. Where the traditional medical model may not be able to explain why two patients with the same injury can have very different pain and disability experiences, the biopsychosocial model accounts for the biological, psychological, and sociological influences that shape the individual pain experience.
Further reading
Massage for Joint Pain: a Biopsychosocial Approach
How Massage Can Treat Chronic Pain

Penny Goldberg, DPT, ATC
Penny Goldberg, DPT, ATC earned her doctorate in Physical Therapy from the University of Saint Augustine and completed a credentialed sports residency at the University of Florida. She is a Board Certified Clinical Specialist in Sports Physical Therapy.
Penny holds a B.S. in Kinesiology and a M.A. in Physical Education from San Diego State University. She has served as an Athletic Trainer at USD, CSUN, and Butler University.
She has presented on Kinesiophobia and differential diagnosis in complicated cases. Penny has published on returning to sports after ACL reconstruction and fear of movement and re-injury.
Outside of the clinic, Penny enjoys traveling, good cooking with great wine, concerts, working out and playing with her dogs.