Chronic pain comes in many different types, including fibromyalgia, complex regional pain syndrome (CRPS), joint pain, and headaches. By definition, chronic pain usually persists more than three months or many months and years. Oftentimes, it is more difficult to treat than acute pain because many factors influence the pain persistence (e.g. immune system, stress, poor mental health).
Massage therapy is among one of several non-drug and non-invasive treatments for some types of chronic pain. While the effects tend to be short-lived (from a few hours to a week), it can help lower the symptoms of anxiety and depression while improving sleep.
Some studies find that massage therapy can reduce a stress hormone called cortisol. However, some more rigorous trials find almost no difference in such hormone levels, which means that there may be other mechanisms that improve mental health and pain that aren’t yet known.
The Center for Disease Control (CDC) reported that about 20% of adults in the U.S. have chronic pain with nearly 7.5% of them having limiting abilities to work and daily activities. Chronic pain sufferers tend to be older adults at 65 and over. However, as many as 20% to 35% of children and teens suffer from chronic pain.
Also, the CDC reported that nearly 24% of non-Hispanic whites are more likely to have chronic pain than:
- non-Hispanic Blacks (19.3%),
- Hispanics (13.0%),
- non-Hispanic Asians (6.8%).
Even though chronic pain is difficult to treat, scientific evidence indicates that treatment and management need many approaches, based on the biopsychosocial model of health.
Different types of chronic pain
Traditionally, chronic pain is boxed in the following types: neuropathic, nociceptive, visceral, psychogenic.
Neuropathic pain
Neuropathic pain is caused by damage or disease in your nervous system whether it’s in your spinal cord, peripheral nerves, or your brain. Most people who have this condition report of having persistent pain or pain that comes and goes that feels burning, pricking, shooting, or clenching. This is usually stimulated by light touch or changes in temperature in the person’s surroundings.
Neuropathic pain is often caused by:
- injuries and accidents
- surgery
- disease (e.g. diabetes, stroke, shingles)
- CRPS
- carpal tunnel
- fibromyalgia
Nociceptive pain
Nociceptive pain usually stems from damage or disease in your tissues (e.g. muscles, skin, joints) where signals from special skin receptors called nociceptors are sent to your central nervous system and brain to process. These nociceptors detect changes and potential dangers in your environment, such as temperature, toxic chemicals, cuts and bruises, and inflammation.
But not all nociception elicits pain and nor does pain require nociception. For example, you may have heard war stories where a soldier has a bullet wound, but they were so intent on getting out of danger that they didn’t notice the wound until they were out of danger. One explanation of how this works is that your pain threshold in your spinal cord is higher than the magnitude of the signals that the nociceptors are generating. When the pain threshold lowers, the signals will transmit to your brain which may or may not give you pain.
Inflammatory pain
Inflammatory pain is a type of nociceptive pain that occurs primarily in your joints, tendons, and ligaments, which causes different kinds of arthritis and rheumatic diseases. Such pain is caused mostly by the interactions of your nervous and immune systems.
Visceral pain
Visceral pain comes from your internal organs and body cavity, such as food poisoning in your gut, gallstones, kidney stones, uterine or ovarian cancer, and diarrhea. Symptoms often include nausea, vomiting, chills, and shakiness of the body.
Somatic pain
Somatic pain is an older term to describe a type of nociceptive pain that involves pain in your limbs. This can be described as an “ouch” pain, like when you stub your toe, get a papercut on your finger, or strain your calf.
Psychogenic pain
Psychogenic pain refers to pain linked to “emotional conflict or psychosocial problems” with no evidence of damage or disease of the nervous system or other symptoms associated with neuropathic and nociceptive pain. This type of pain is often associated with depression, anxiety, PTSD, chronic stress, and various psychological disorders that change how the brain and the nervous system perceive pain.
Therefore, clinicians must understand the social, psychological, and biological factors that contribute to psychogenic pain. Keep in mind that some researchers and clinicians no longer use the term “psychogenic pain” because it’s considered outdated and stigmatic, bringing back the days when people with mental health problems were labeled as having “imaginary pain.” Thus they often were not given proper treatment and care and were mostly ignored.
Why categorizing types of pain can be problematic
Categorizing people with a type of pain isn’t “cut and dry,” as licensed massage therapist Mia Plukett said, who is a private practitioner in Little Rock, Arkansas, for about 15 years. In some cases, there are just too many overlaps of each category to define the type of pain someone has.
“I think often when practitioners are discussing chronic pain, they use it as shorthand for people with unspecified pain,” she said. “These are people for whom no bloodwork or anatomical cause has been found as a “cause” for their pain.”
For example, a client of hers had stage IV breast cancer, degenerative disc disease, symptoms from taking radiology medications, new onset of neuropathy in their limbs, and intense low back pain. So do they now have nociceptive pain? Nociplastic pain? Or neuropathic?
“The case took four medical doctors more than six months to figure out. They had a fractured sacrum and ilium with radicular pain exacerbated by their medication,” Plunkett said.
“Or, what about the case of chronic unexplained pain and eventual foot drop that was later diagnosed as ALS?” She described another case of hers. “They were referred to psychiatry three times prior to their ALS diagnosis. It was four years looking for a diagnosis with many other misdiagnoses along the way prior to their ALS diagnosis. Was their pain less central prior to their diagnosis? Many neurological or autoimmune conditions take years to diagnose properly. Even with a diagnosis, syndromes overlap.”
“I think the bottom line has to be for us as clinicians to keep an open mind, to believe the person in front of us. They really do know their bodies better than we do,” Plunkett continued. “As clinicians, we get biased, too. We think we know what’s ‘causing’ someone’s pain after meeting them for 50 minutes or less. I think it’s rarely so simple. While [categorizing pain] is important and helps us organize our thoughts and treatments—and for those who do so, our diagnostics—remember that real life is rarely so neatly laid out.”
Can massage therapy help with chronic pain?
Massage therapy can reduce pain temporarily by changing how your nervous system processes pain. Under your skin, there are several types of nociceptors that detect stimuli from your environment. Whether the stimuli is from a massage, a hug, or someone poking your back with their finger, these skin receptors can affect how you experience pain and pleasure.
- Aδ fibers: responds to hard or sharp pressure, such as on a crushing grip or piercing thorn. They also function as proprioceptors, sensing where joints and other body parts are located within your personal space.
- C fibers: responds to temperature and chemical stimuli, such as heat, cold, and acids.
- Aβ receptors: responds to light touch, such as a brush from a feather or a gentle caress. They can also inhibit nociceptive input from Aδ and C-fibers.
So theoretically, massage therapy “activates” Aβ receptors while inhibiting signals from other fibers. It’s also likely that massage can improve other parts of your life that can reduce your pain, such as better sleep, increase in exercise frequency, and higher self-efficacy.
But massage therapists provide more than just touch to reduce pain. A good therapeutic relationship with a therapist can also be beneficial for you since they are acting as a support.
“I think people with chronic pain come to massage therapy for all kinds of reasons,” Plunkett said. “Massage therapists don’t diagnose patients. We simply listen to the diagnostics they bring to us and make our own (internal) assessments from that starting point. This is a real strength of the massage profession as it’s not within our scope to add on additional ‘problems’ or diagnostic-like proclamations concerning a person’s ‘cause’ of pain. What we do beautifully is listen to people, validate their whole experience(s), and act as a reflection for them.”
Plunkett added that massage therapists can be their clients’ or patients’ partners in their care, similar to some healthcare professionals. “We can simply be reliable health care providers offering a safe, judgment-free space for healthy touch. I think that last bit is vastly underappreciated, but so important,” she said.
Symptoms of chronic pain
Chronic pain symptoms vary, such as achiness, burning pain, weakness, and fatigue. Some of these symptoms can be felt all over the body (e.g. fibromyalgia and CRPS) while some are more localized, such as
- irritable bowel syndrome (IBS)
- pelvic pain
- low back pain
- neck pain
- shoulder pain
- migraines
- jaw pain
Oftentimes, the pain intensity can go up and down throughout the day or week, and it can be dormant for a certain amount of time.
Causes of chronic pain
Much of the current body of research indicates that there is no single cause of chronic pain. Based on the neuromatrix theory of pain, which is widely accepted for explaining and understanding pain, both acute and chronic pain are influenced by biological, cognitive, and emotional factors.
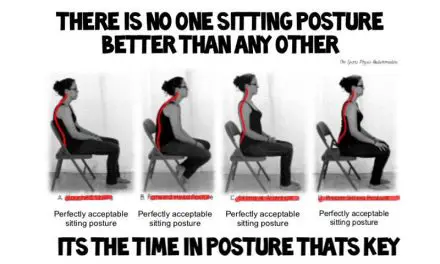
Traditionally, many clinicians thought (and many still do) that muscular and joint pain stem from a single or a few causes if there’s no disease or injury detected. Such causes include “poor” posture, faulty movement patterns, leg-length discrepancy, tight muscles or fascia, or weak core muscles.
Pain researchers currently understand that biological and biomechanical factors are not the ones that influence chronic pain. They may or may not matter, but they are still a small piece of the bigger pain puzzle. Whether it is neurological, inflammatory, nociceptive, or phantom limb pain, pain also is affected by our thoughts, emotions, and environment.
For example, racial discrimination, economics, and gender can affect the likelihood of developing chronic pain among adults and during childhood or adolescence that carries into adulthood. Given the current evidence about chronic pain, clinicians should not say that “you’re imagining it” or “it’s all in your head.” If anyone says that to you, find another healthcare professional who understands your needs and takes time to listen to you.
Risk factors to chronic pain
The most important risk factor for chronic pain is pain (acute or chronic) at another site. In fact, people with more severe pain or pain in multiple areas are more likely to develop severe chronic pain. Other risk factors associated with chronic pain can be modifiable or non-modifiable.
Modifiable risk factors
- pain
- mental health
- smoking
- alcohol
- obesity
- physical activity
- sleep
- nutrition
- employment status
Non-modifiable risk factors
- age
- gender
- cultural background
- socioeconomic background
- history of trauma/injury/violence
- genetic factors
Central sensitization
Central sensitization is associated with the development and maintenance of chronic pain through the nervous system. When this process occurs, the nervous system is in a heightened state of reactivity which lowers the threshold for pain perception and pain maintenance regardless of whether the initial injury is still present. In other words, you’re more likely to experience pain from a stimulus that wouldn’t cause such pain for people without central sensitization.
In acute pain, the sensory receptors in your skin send a message along the pain-sensing nerves to the spinal cord and brain where the sensation is then registered, processed, and finally, the pain is perceived.
In chronic pain, this process can be disrupted in two ways: allodynia and hyperalgesia. In allodynia, pain is perceived with things that are not normally painful. This could be as simple as light touch or even the feeling of clothes on your body. Because the nervous system is already on red alert, the brain produces a sensation of pain and discomfort rather than the mild sensation of touch.
In hyperalgesia, something that is typically painful is even more painful than it should be. A typical example of this might be an ordinary bruise that should be mildly painful but instead is felt as severe pain. Again, because the nervous system is already sensitive, the pain sensation is amplified.
Treatment of chronic pain
You may run into the gamut of medication, psychotherapy, physical activity, or even surgery for treating chronic pain. It may take a frustratingly long time to find the treatment that works best for you.
Stress management
Stress management encompasses several strategies that relieve stress. For some people, this could be a warm bath while others prefer to take a walk. Breathing exercises such as those taught in yoga or meditation can also help calm the mind and body.
Sleep
Sleep is a wonder “drug.” Some techniques, such as making sure you only sleep in your bed, not watch TV, read, or play on your phone, can help you get a better night’s rest. Having a mattress that is comfortable and a cool room can also improve sleep quality.
Food and drink can also make it difficult to sleep. Avoiding spicy foods and caffeinated drinks within five hours of bedtime is a good general rule of thumb to follow when trying to maximize sleep time.
Exercise
One of the easiest ways to feel better is to move your body. Exercise causes your brain to release endorphins which can be natural pain relievers (you can also increase endorphins through listening to your favorite song or eating chocolate!). Choosing low-impact activities that move your joints through their full range of motion, such as tai chi, yoga, or aqua aerobics, can be a good place to start your journey to pain relief through exercise.
Diet
It’s more difficult for your body to process processed foods than whole food. Eating more fruits, vegetables, and lean protein sources can help give your body the fuel it needs to get through the day. Foods that are high in salt, sugar, and fat tend to cause energy levels to plummet.
It’s also critical that you stay hydrated! Being well hydrated can help with digestion, brain performance, energy levels, weight management, temperature regulation, and joint pain.
Social activities: Maintaining your social life and friendships can help stabilize your mood. Interacting with friends and family can combat feelings of depression and isolation. You may need to prioritize these activities on ‘good days’ or consider pacing yourself when it comes to planning outings. Your ‘not so good days’ are a great time to let friends and family come visit you.
Spinal cord stimulation: Spinal cord stimulators are small, implantable devices that send electrical signals to the brain to relieve pain. Spinal cord stimulators are typically reserved for patients who have failed less invasive therapies such as physical therapy, massage therapy, injections, oral medications, and rhizotomy.
These devices can be quite helpful but implantation and maintenance of the devices can be very cumbersome. Conventional spinal cord stimulators eventually run out of battery life requiring another surgery to implant a new battery. Newer technology offers rechargeable devices that also give off more electricity which may be helpful in patients who have pain in multiple areas.
Other surgeries
Surgery is typically a last resort for chronic pain unless there are neurological complications (bowel or bladder dysfunction). In order to be a candidate for surgery to address your chronic pain you should meet two criteria:
1) have failed all conservative therapies;
2) have an identifiable source of pain.
If those criteria are met, some surgical procedures that may be considered include dorsal rhizotomy/radio-frequency ablation, microdiscectomy, peripheral nerve surgery, or joint replacement.
Cognitive behavioral therapy (CBT)
Cognitive behavioral therapy is a proven approach for treating a variety of conditions including chronic pain, depression, anxiety, relationship problems, substance abuse, and eating disorders.
The core idea of CBT is that most of our problems stem, in some part, from unhelpful thinking and behaviors. Learning coping strategies that address the unhelpful thinking and behaviors can lead to pain relief and improved quality of life.
CBT involves learning to face your fears rather than avoid them, calm your mind and relax your body, and develop confidence in your own skills and abilities.
Physical therapy
Physical therapy is a great option for learning to manage your chronic pain. The therapist can help you find exercises that maximize strength and range of motion while building endurance to participate in the things you love.
When you practice pain-free exercises you teach your body that movement is safe and non-painful which leads to moving in bigger ranges, for more time, with less pain. Physical therapy can also teach you to modify exercises and how to pace yourself through daily activities to avoid a crash.
It may also involve massage, soft tissue manipulation, breath work, or electrical stimulation to help with pain management.
Occupational therapy
Similar to physical therapy, the goal of occupational therapy is to get you back to doing the things you need to do or enjoy in your life. Occupational therapy focuses on using adaptive techniques or equipment to perform daily activities.
Working with an occupational therapist can teach you coping and pain-management skills and improve function and quality of life. Some of the strategies include: sleep improvement, eating and exercise routines, activity pacing and energy management, ergonomic training, community involvement and participation in social activities, and self-regulation strategies for managing daily stress as well as flare-ups.
Psychotherapy
Psychotherapy is typically referred to as talk therapy. There are several techniques that fall under this umbrella. The types of therapy that seem to be most helpful for pain include CBT, acceptance and commitment therapy (ACT), mindfulness, or biofeedback.
Therapy can help with the mental anguish of constant pain. Depression, fear, anger, stress, and anxiety have all been associated with chronic pain.
Psychotherapy can be a useful adjunct in pain management because these emotional responses can lead to more pain. Learning to manage the negative thoughts, feelings, and behaviors that surround chronic pain through meditation, relaxation, goal setting, and graded activity exposure can help improve quality of life.
Can I live well with chronic pain?
Despite having chronic pain, some people are able to cope and live an independent life. They are able to make a living, participate in activities and gatherings, and seek little to no treatment.
Researchers in New Zealand, led by Dr. Bronnie L. Thompson from the University of Otago, found that the people in their study who were able to regain their sense of self and resume their occupation are able to cope with their chronic pain. They theorized that people are able to cope by “achieving self-coherence by engaging in the process of re-occupying the self” through their jobs. In other words, they took control of their lives instead of letting their pain do so.
Their sense of self is described as “the direct feeling each person has of privileged access to his or her own thoughts, feelings and sensations.” Without this, they risk losing their self-worth and their role in society before they have chronic pain.
Thompson wrote that they have noticed a smaller group of people with chronic pain who seem to be coping well. “They’re active, maintain going to work, keep the family going and so on,” she wrote. “But at the same time [they] can be highly distressed by their pain. Their pain represents a roadblock that gets in the way of getting things done.”
Instead of giving up and doubling down on the chronic pain, these people “almost redouble their efforts” to find ways to keep doing what they are doing. For one of Thompson’s subjects, who suffered from chronic pain for more than 10 years, she found a renewed purpose to her role with her family and community.
“When I began doing what matters to me, maybe in a different way but still doing them, I felt more myself again instead of this alien within my skin,” she said.
Takeaway
Chronic pain can be daunting and debilitating, but it doesn’t have to be. Finding the right team of physicians, therapists, and other support arms can give you proven strategies to navigate this very bumpy, windy road. As difficult as it may seem, continuing to engage with the outside world and your friends and family is an important part of the treatment for chronic pain.
You’re not alone in this journey. Aside from your care team, there are also several online resources and support groups available.
- Pain Connection offers national support groups that meet via Zoom several times a month.
- Psychology Today is another great resource that offers a tool to find in-person groups near you.
- The U.S. Pain Foundation website offers several publications related to chronic pain as well as educational seminars and countless support group options that are both in-person and online.