There are many shoulder tests that can help rule in or rule out a rotator cuff tear. These include:
- Drop arm test
- Belly press test
- Lift off test
- Empty can test
- Full Can test
- Hornblower’s test
- Bear hug
Physical therapists use these tests based on the size, location, age, and condition of the tear as well as the patient’s fitness level and age.
Typically, a cluster of tests is the best way to determine if the rotator cuff is torn because a positive test in one patient may be negative in another, even if they both have tears. And so, using the cluster of tests helps increase the likelihood that the findings are correct.
Types of rotator cuff injury tests
Rotator cuff tests are grouped by the muscle being tested or the diagnosis being ruled in/out. In most cases, a single test is not enough to confirm a diagnosis.
Drop-arm test
The Drop-arm test is used to diagnose full-thickness rotator cuff tears.
To perform the test, the therapist passively abducts the patient’s arm to 90 degrees with full external rotation (thumb up position) and then asks the patient to hold this position as the therapist withdraws support.
If the patient can not hold the arm at 90 degrees, the test is positive.
Bear hug test
The bear hug test examines the main internal rotator of the shoulder, the subscapularis.
The test starts with the patient placing the palm of their involved side on the top of their opposite shoulder. The patient is asked to hold this position while the therapist pulls the patient’s forearm away from their body.
If the patient cannot hold their hand against their shoulder, the test is considered positive.
Lift-off test
The lift-off test (also known as Gerber’s test) is used to detect a subscapularis tear. The test is often performed in standing but the patient can be sitting as well.
The patient is asked to place the involved arm on the small of their back with their palm facing outward. If they can achieve this position, they are asked to lift their hand off their back.
The inability to lift the hand off their back is a positive test. Also, the inability to achieve the test position doesn’t indicate a positive test, only that a different test may be more suitable to the patient.
Belly press test
The belly press test is used to determine if there’s a tear in the subscapularis muscle. This can be a good alternative to the lift-off test for patients who are unable to get their arm behind their back.
The patient bends their elbow to 90 degrees so that the palm of their hand is on the upper abdomen (just below the breastbone). The patient presses their hand against their abdomen to create relative internal rotation.
The test is positive if the patient cannot perform this task. In some cases, the most common compensatory movement is where the elbow on the involved side moves closer to the patient’s body.
Empty can test
The empty can, or Jobe’s test, is used to examine the supraspinatus muscle. The patient raises their arm to 90 degrees in the scapular plane (about 30 degrees to the outside of a front raise) with their elbow straight and the thumb pointing down as if they were emptying a can.
The therapist applies downward pressure at the wrist while the patient tries to maintain their position.
The test is positive if the patient cannot hold the position or has pain when resistance is applied.
Ultrasound scans
Ultrasound has gained traction in the rehab world over the last decade. Although the technology has been around for quite some time, it has become more affordable for most clinics recently. This type of ultrasound may be used by a physician, radiologist, or physical therapist.
Farooqi et al. performed a systematic review and meta-analysis of the use of diagnostic ultrasound in patients with rotator cuff tears.
The studies looked at over 2,000 shoulders and found that ultrasound was better at detecting tears in the supraspinatus and biceps tendons than the subscapularis tendon. Ultrasound also shows more diagnostic accuracy for full-thickness than partial-thickness tears.
When compared to magnetic resonance imaging (MRI), there was no difference in the ultrasound’s ability to reveal rotator cuff tears. Regardless of which method is used, what’s more important is that a tear is present as it has the potential to lead to other problems down the road.
What does a torn rotator cuff feel like?
Most patients with rotator cuff tears will report pain, limited motion, and weakness in their shoulder.
Patients with rotator cuff tears may or may not know when the injury happened. Some describe very painful experiences when lifting something while others have pain that comes on over time. There can be painful or non-painful clicking or clunking that accompanies a tear as well.
When the rotator cuff is torn, a deep, aching pain tends to develop in the shoulder and upper arm.
The tear may be mistaken for a deltoid strain in a less experienced clinician because those with a rotator cuff tear describe pain on the outside of their upper arm about a third of the way from the shoulder to the elbow. They may also have aching pain in their elbow.
Reaching the arm overhead or out to the side and sleeping are typically the top two functional limitations these patients report, but they may also have difficulty with driving, dressing (specifically tucking a shirt into the back of their pants or fastening a bra behind the back), or exercise. These patients may also present with a ‘painful arc’ meaning they have pain through the mid-range of motion.
Rotator cuff injury treatments
Despite what most people think, surgery is not the only treatment for rotator cuff injury. Non-invasive options, such as physical or massage therapy, corticosteroid injections, prolotherapy and taping are often the preferred first-line treatment for a rotator cuff tear.
The International Journal of Sports Physical Therapy published a systematic review of non-operative treatment for rotator cuff tears in 2018. The review examined over 1,500 unique citations and included over 2,000 shoulders.
Based on the studies, nearly 80% had improvements in pain, more than 80% had improved range of motion, 85% were able to regain strength, and 84% reported functional improvement.
A mere 15% failed conservative therapy and went on to have surgical repair of their rotator cuff tear.
Rotator cuff stretches
Stretching a torn rotator cuff may not be possible in the early stages of injury because of pain. Once the initial pain has settled, these patients often have limited internal and external rotation.
Stretches that address these motions can help restore muscle length so that the patient can focus on strengthening through their full range of motion.
Physical therapy
Physical therapy for a rotator cuff tear should include work to restore range of motion and flexibility as well as improve strength and endurance of the rotator cuff and surrounding musculature.
Manual therapy and electrical stimulation can be used to decrease pain and improve range of motion. Emerging treatments, such as blood flow restriction training and dry needling, may also be used as adjuncts to more traditional therapy techniques.
Rotator cuff surgery
Surgical repair of the rotator cuff may be necessary. The extent of the surgery (and subsequent rehabilitation) depends on the size of the tear.
Following surgery, the shoulder is immobilized to allow the repair to “take” and then a physical therapist guides and helps the patient restore their range of motion and strength.
A 2017 study looked at operative versus non-operative treatment of rotator cuff tears. The review included 269 patients who were at least one-year out of surgery.
Results showed that statistically, patients who had surgery had better subjective and objective outcomes but these differences were too small to be clinically meaningful.
KT tape
As with most other conditions, the reviews on whether kinesiology tape (KT tape) and other types of tape works or not are mixed. Although the tape is unlikely to truly change muscle activity or strength, it may have other benefits for shoulder pain and function.
Applying KT tape to the skin can improve proprioception—your body’s ability to know where it is in space—which may be lost when the rotator cuff is torn. And so, improving proprioception can lead to improved mobility and stability of the shoulder joint.
How taping works may be as simple as how it is explained to the patient.

Taping may improve an athlete’s proprioception, but so far, there’s not much research to show how taping works so. (Photo by Penny Goldberg.)
Akbaba et al. examined the influence of verbal cueing when they used Kinesio Tape in patients with a rotator cuff tear.
Eight-nine patients were separated into three groups who were each given different information about whether or not the tape works.
The patients in the group who were told the tape had limited or excellent support had decreased pain at rest for 30 minutes after they were taped.
But in the group that was told the tape had excellent support, the pain relief lasted through the first 24 hours.
Rotator cuff exercises
Rotator cuff exercises focus on strengthening the muscles that perform internal and external rotation of the shoulder, and the list of options for how to do this is nearly endless.
That said, when someone says “rotator cuff exercises” most people think of those done with an elastic band that is connected to a wall or the hinged side of a closed door. Once the band is secured, the patient squeezes a towel between the elbow and their rib cage while the band creates resistance in the appropriate direction.

The typical rotator cuff exercise is one out of many that you can do to strengthen the rotator cuff muscles. (Photo by Penny Goldberg.)
In reality, there are tons of exercises with hundreds of variations that address the rotator cuff muscles and those that support it. Among these include:
Overhead press
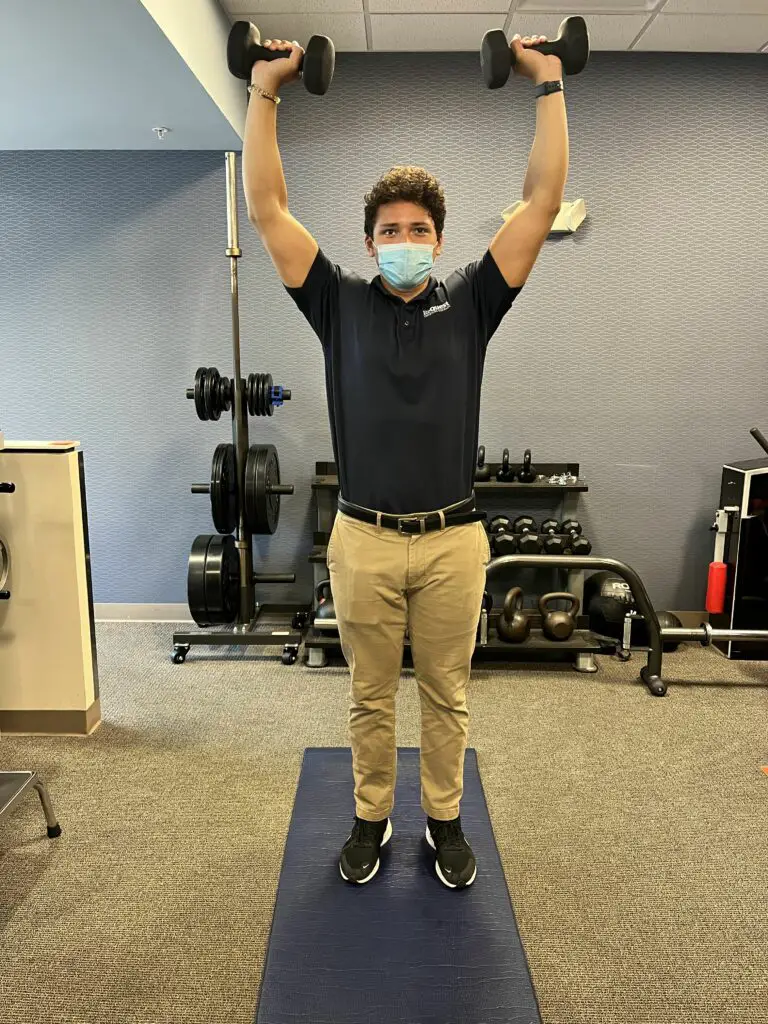
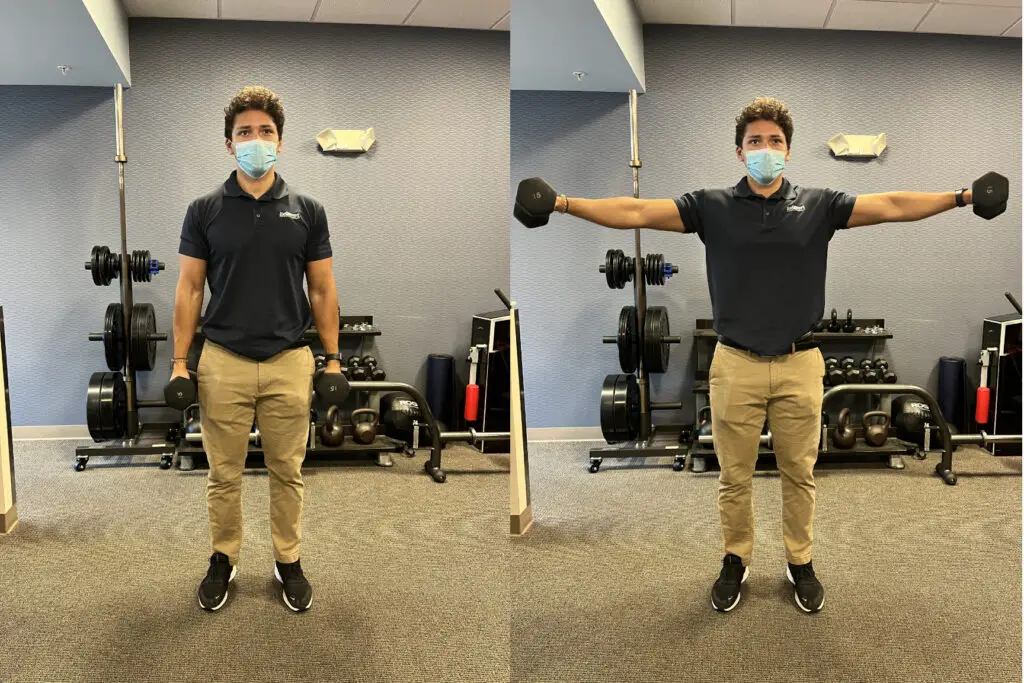
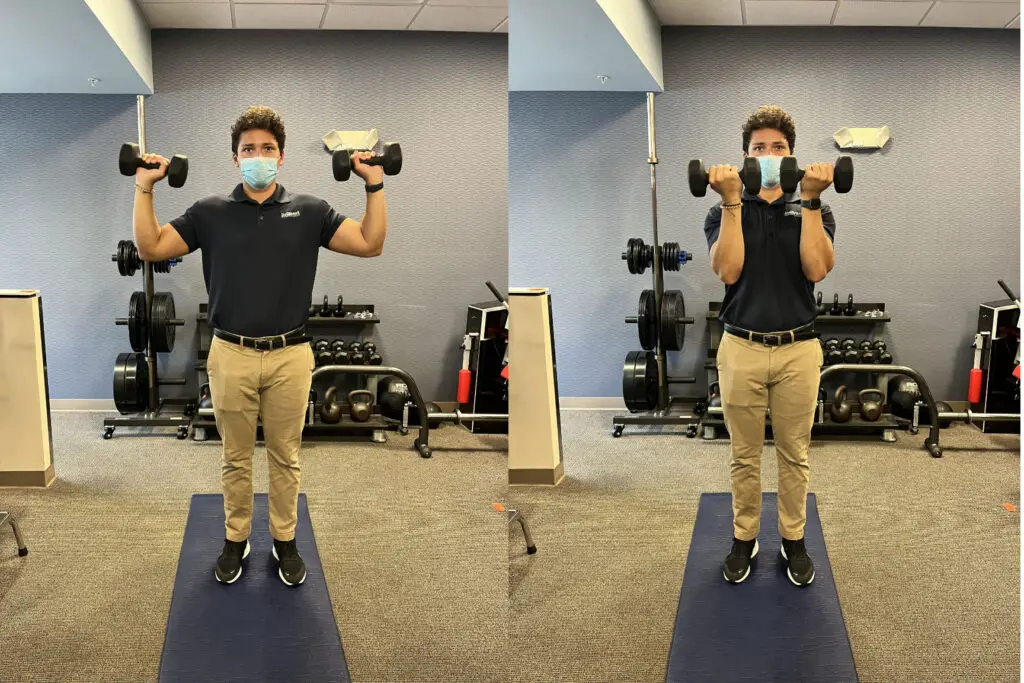
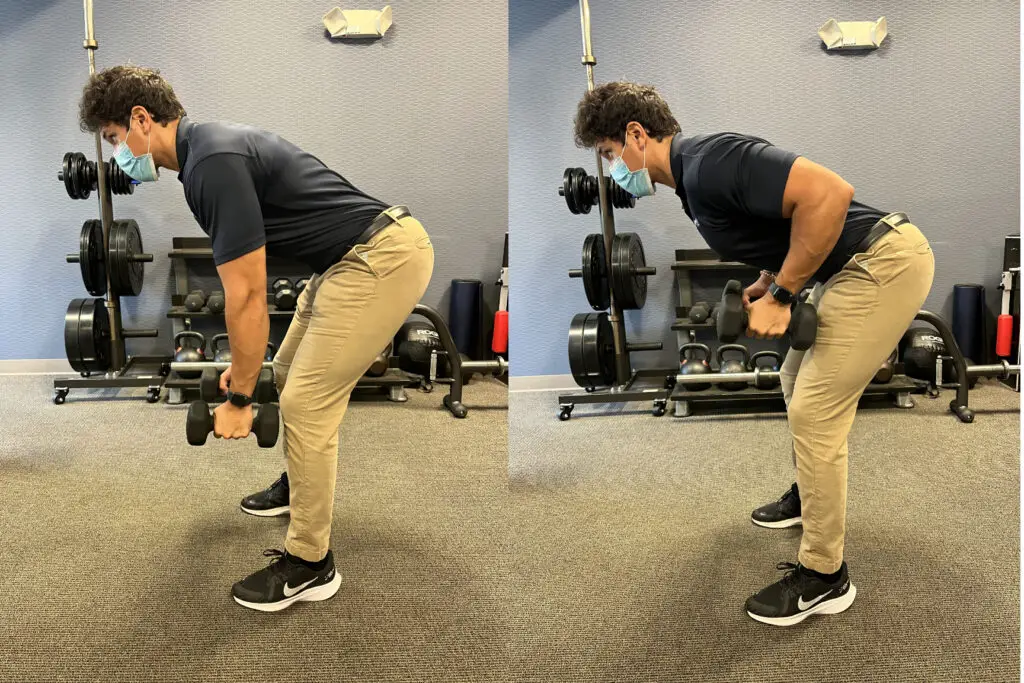
(Photos by Penny Goldberg.)
Lateral raise
Arnold press
Dumbbell back row
Some researchers suggested that patients with symptomatic rotator cuff tears should start with exercise-based physical therapy, but the specific exercises and training loads that should be used have not been established. This may boil down to each patient’s condition, ability, and preference of exercise.
Teixiera and colleagues reviewed the role of scapular function in rotator cuff tears and suggested that symptomatic rotator cuff tears should start with exercise-based physical therapy, but the specific exercises and training loads that should be used have not been established.
How long after a rotator cuff surgery can you drive?
This is a very popular question that’s very difficult to get a straight answer. Most physicians will allow a patient to drive when the following criteria are met:
- They are no longer taking pain medications
- They are no longer wearing a sling or other motion-restricting device
- They can safely control the car
Deciding when you can safely control a car is the difficult part of the question; most patients can drive with their non-surgical arm only but that may not be the safest option.
A 2022 study investigated the ability to drive after rotator cuff repair. Researchers evaluated several driving tasks and maneuvers on a 15-mile course that took 45 to 55 minutes to complete.
Participants were tested at 2, 4, 6, and 12 weeks after surgery. Researchers determined that patients were able to drive safely as early as two weeks after undergoing a rotator cuff repair.
As said earlier, not all rotator cuff tears are the same, and so, not all rotator cuff surgery is the same. The location, size, and extent of the tear as well as the age and overall health of the patient can influence how well they recover and function.
When “can I drive?” is posed to me in the clinic I often respond with a couple questions of my own: Can you turn the steering wheel in both directions without pain using either hand? Can you maintain the “10 and 2” position for a prolonged period of time without pain?
Can a torn rotator cuff heal naturally without surgery?
Unfortunately, a torn rotator cuff doesn’t “heal” without surgery. However, you don’t always need 100% of your rotator cuff to be intact to have full, pain-free use of your shoulder.
Although the tear will remain, shoulder mobility, flexibility, strength, and endurance can be restored so that the tear is no longer noticeable in your daily life. Clinically, we would refer to the tear as “asymptomatic” rather than healed.
There may be times where the tear becomes symptomatic or ‘flares up,’ but these can likely be addressed through the PT exercises that have been previously learned.
Rotator cuff pain and massage therapy
Patients with rotator cuff tears may have limited mobility which can interfere with positioning during massage therapy. These patients may have difficulty lying with their arm over their head or at their side when face up.
Dr. Alex Moon, who is a physical therapist and a licensed massage therapist based in Phoenix, Arizona, suggests that the first thing a massage therapist should do with a client that has a rotator cuff tear is assess motion.
“Ask the patient to move their shoulder into flexion, abduction, external rotation and internal rotation to get an idea of how the patient is moving,” he said.
Moon then uses the information to prioritize which muscles he will target with his hands-on work. If the patient has back pain while lying on their back, the humerus dropping below the midline of the body is likely the pain generator.
“It may be necessary to use a rolled up towel under the patient’s elbow to prop [the arm] up,” Moon suggested.
Rotator cuff tears can be asymptomatic. While these patients may not have overt signs of injury, a skilled massage therapist will likely find areas of pain and limited motion that the patient may not have been aware of.
Also, rotator cuff injuries can wreak havoc in other areas of the body, thanks to something called “regional interdependence.” Although a person can fully function with a rotator cuff tear, they may do so with extra help from other body parts. Moon advocates looking at the muscles around the shoulder blade and throughout the back for tightness that might be affecting the shoulder.
“[Massage therapists] may be the first person to catch compensation patterns on the opposite side of the body or reactionary patterns such as jaw clenching and neck stiffness in response to pain,” he said.
As a sports physical therapist, I see a lot of rotator cuff tears. A LOT. This diagnosis and type of shoulder pain is far more common than you think. If I had a nickel for every time I’ve seen fear in a patient’s eyes when I’ve said, “I think you have a rotator cuff tear,” I probably wouldn’t have to work anymore.
Once we get past the patient’s fear of the diagnosis meaning surgery, we can move on to talking about all of the non-invasive options that are available to address their pain and dysfunction and effectively heal the rotator cuff naturally.
Further reading
How Massage Can Treat Chronic Pain
Descending Modulation: Why Massage Therapy Can Help Alleviate Pain
Massage for Joint Pain: A Biopsychosocial Approach

Penny Goldberg, DPT, ATC
Penny Goldberg, DPT, ATC earned her doctorate in Physical Therapy from the University of Saint Augustine and completed a credentialed sports residency at the University of Florida. She is a Board Certified Clinical Specialist in Sports Physical Therapy.
Penny holds a B.S. in Kinesiology and a M.A. in Physical Education from San Diego State University. She has served as an Athletic Trainer at USD, CSUN, and Butler University.
She has presented on Kinesiophobia and differential diagnosis in complicated cases. Penny has published on returning to sports after ACL reconstruction and fear of movement and re-injury.
Outside of the clinic, Penny enjoys traveling, good cooking with great wine, concerts, working out and playing with her dogs.






