Shoulder bursitis is an inflammation of the bursa, a small fluid-filled sac in the shoulder joint that acts as a cushion between the bones and soft tissues. A bursitis occurs when the bursa becomes inflamed and irritated. This can lead to pain, swelling, and reduced range of motion in the shoulder.
This article covers whether massage therapy and exercise could reduce shoulder bursitis symptoms.
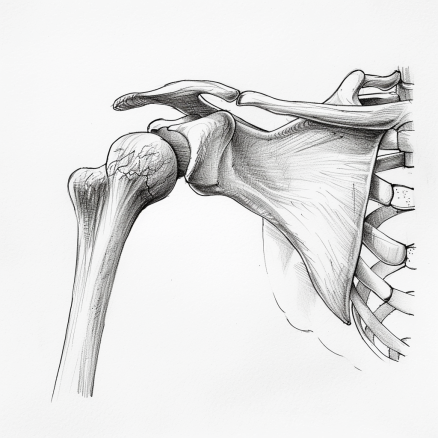
Shoulder bursitis anatomy
There are four major shoulder bursae and two minor ones in the shoulder area.
Sumacromial bursa
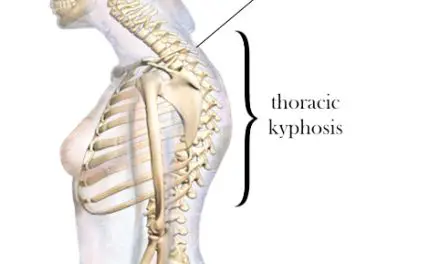
The subacromial bursa, which is more prone to shoulder bursitis than other bursae for some populations, is located deep within the subacromial space of the deltoid, sandwiched between the acromion, the coracoid process, the coracoacromial ligament above it, and the supraspinatus muscle below. It is also bordered to the side by the deltoid muscle.
Sub-deltoid bursa
The subdeltoid bursa, which is often grouped with the subacromial bursa, extends toward the deltoid muscle from the subacromial bursa.
Subscapular brusa
The subscapular bursa is a flat, irregularly shaped bursa located between the subscapularis muscle and the scapula. Its definition and anatomy remains somewhat controversial because some researchers consider it a separate pouch, while others believe it’s actually the superior subscapularis recess, which is an outpouching of the glenohumeral joint capsule.
Subcoracoid bursa
The subcoracoid bursa is located to the front of the subscapularis muscle and below the coracoid process. It reduces friction among the short head of the biceps brachii tendons, subscapularis muscle, and the coracobrachialis.
Nerves that innervate the subacromial bursa include the free nerve endings that stem from the axillary nerve of the brachial plexus at the armpit. Some studies have shown that the subacromial bursa is innervated by the branches of the suprascapular nerve and the lateral pectoral nerve.
In this article, shoulder bursitis refers to the subacromial bursa unless stated otherwise.
Shoulder bursitis symptoms
Symptoms of shoulder bursitis include:
- Pain on the outer side of the shoulder, which can be mild at first but gradually increase over time and may be felt even at rest
- Pain that intensifies after repetitive shoulder movements or activities, such as overhead lifting, throwing, or playing sports
- Shoulder tenderness and sensitivity to pressure, making it uncomfortable to lie on the affected side
- Radiating pain down the outside of the arm, though rarely past the elbow
- Muscle weakness as the person avoids using the shoulder, causing the muscles to weaken
- Difficulty reaching behind the back or overhead due to pain and reduced range of motion
- Lack of notable swelling, as the bursa typically only thickens slightly (around 0.5 mm)
- Septic bursitis may yield additional symptoms, such as fever, fatigue, and warmth/redness at the shoulder site
Sometimes shoulder bursitis shares symptoms with shoulder impingement, such as inflammation of the rotator cuff tendons which causes them to thicken.
Shoulder bursitis causes
Shoulder bursitis pain is often caused by several factors, rarely just one.
Overuse and repetitive overhead movements
Athletes and workers who perform repetitive, overhead movements with their shoulders may likely increase their risk of getting shoulder bursitis. Among athletes, they include those who play volleyball, tennis, badminton, baseball, and football (particularly the quarterback).
Overhead throwing requires having enough relaxation of the shoulder to allow as much external rotation as possible to prep the throw and then produce enough speed and force to perform the throw while stabilizing the joint.
Infection
Bursitis could be caused by septicemia, or blood infection, by bacteria. Septic bursitis likely come from invasive procedures like surgery and injections.
Like frozen shoulders, injections to the shoulder may increase the risk of such infections, and it is likely these bacteria are not the only ones. One retrospective study published in 2017 found that Staphylococcus aureus is the most common type of bacteria to contribute bursitis and pain in the elbow and knee after the joint is injured.
In rare cases, the bacteria that cause meningitis, such as Neisseria meningitidis, has been shown to infect the ankle of a 72-year-old woman in Japan in 2017. Other types of bacteria has been found to infect different bursae, but these are quite rare.
While nearly all major research focuses on the elbow and knee bursae, it is unknown whether Staph bacteria is a major contributor to shoulder bursitis.
Inflammation
Inflammation of the nerve endings of the bursae can be caused by infection, overuse of repetitive movements of the shoulder, injury, or a combination of these and other factors. Research has shown that people with shoulder pain from shoulder bursitis have elevated levels of cytokines and neurotransmitters, such as interleukins and P substance.
Interleukins are a type of cytokines that are part of a specialized group of proteins that are vital in cell communication during an immune response. P substance is a type of neurotransmitter that is located mostly in the primary afferent nerves and is partly responsible for transmitting messages that stimulate the nerve endings to the brain.
Asymptomatic shoulder pain
Some studies have found that patients with signs of shoulder bursitis, lesions in the rotator cuff muscles and tendons, and other shoulder “abnormalities” do not experience pain. In a 2014 systematic review, researchers from Harvard Medical School examined 30 studies (over 6,100 shoulders total) that reported rotator cuff abnormalities with age. They concluded that it is “considered a common aspect of normal human aging” and difficult to conclude whether the abnormalities are fresh or a cause of shoulder pain.
[Related: Shoulder “Abnormalities” May Not Always Be a Cause of Pain or Disability]
There’s little research on asymptomatic cases of shoulder bursitis itself, but clues from other types of asymptomatic shoulder conditions indicate that it is likely to have bursitis without feeling pain. One study of 51 men and another study of 305 women with asymptomatic shoulders found various types and degrees of shoulder abnormalities, including thickening of the subacromial bursae and calcification in the rotator cuff muscles.
Shoulder bursitis prognosis
While there is a lack of a body of research behind the prognosis of shoulder bursitis, it’s possible to draw some clues from other types of shoulder pain.
Psychosocial factors have been shown to affect how well patients recover from chronic shoulder pain. For example, a team of Spanish and Belgian researchers found that patients with high levels of self-efficacy, resilience, and expectations of recovery were “significantly associated with low levels of pain intensity and disability.”
Not surprisingly, patients with high degrees of depression, anxiety, pre-operative concerns, fear-avoidance beliefs, and emotional distress had higher pain intensity and disability. The systematic review is based on 27 longitudinal studies with a sum of more than 11,100 subjects.
In 2018, the first systematic review of psychological factors and rotator cuff tears also found similar relationships as the aforementioned study, based on five prospective cohort studies and five cross-sectional studies with a total of 1,410 subjects. Interestingly, what the researchers found is that the correlation between rotator cuff pain and most psychological factors, such as depression and anxiety, are “weak to moderately correlated with patient-reported outcomes at the preoperative time point.” In other words, there was not much of a significant relationship between how they felt and how much pain or disability they had before they underwent surgery.
Patients’ expectations about the surgery was reported to be the biggest psychological factor in driving surgical outcomes, but these were reported in three of the five cohort studies.
About two years later, a similar systematic review from the University of Hong Kong also found similar results about rotator cuff pain and tendinopathy and psychological factors. Researchers Wong et al. found that one-fourth of the patients had “depressive and anxious symptoms,” and nearly 90% of the patients had insomnia.
What all three of these reviews have in common is that the quality of the studies included were mostly quite low because of inconsistent ways of setting up the experiment, reporting bias, publication bias, small number of studies included, and other limitations.
Shoulder bursitis diagnosis
There are no universally accepted diagnostic criteria, but the combination of characteristic symptoms, physical exam findings, and imaging results are typically used to diagnose subacromial bursitis.
Patients’ clinical history forms the foundation of a diagnosis for shoulder bursitis. For example, patients with shoulder bursitis may likely have pain in the upper arm and sometimes radiate to the wrist. A physician or physical therapist would likely perform differential diagnoses to rule out other potential causes, such as fractures, calcification of the shoulder bursa, osteoarthritis, and shoulder dislocations by using different types of scans.
For manual testing, there’s not much evidence to determine whether patients have shoulder bursitis or not. Even if it’s detected with imaging, bursitis is not always an indicator of shoulder pain.
Tests for shoulder impingement would likely be used by orthopedic physicians or physical therapists. These would include the painful arc test, Neer’s test, and Hawkins-Kennedy test.
A 2014 Cochrane Review of 33 qualified studies found that there is “insufficient evidence upon which to base selection of physical tests for shoulder impingements” and other lesions in the tendon, labrum, or bursa that often accompany shoulder impingements. The researchers pointed out that most of the studies were of poor quality since many of them have different methods to test the manual tests and different population samples.
Shoulder bursitis treatment
As with most types of joint pain, most physical therapists and other healthcare professionals would likely have you try conservative treatments before considering surgery as the last option.
Medications
Oral medications, such as non-steroidal anti-inflammatory drugs (NSAIDs), may initially help reduce pain, but they have side effects for some people, such as gastrointestinal problems. Researchers Justin Tien and Andrew Tan from Singapore General Hospital suggest that NSAIDs should be taken no more than two weeks, but check with your physician or a qualified healthcare provider for your specific dosage and treatment duration.
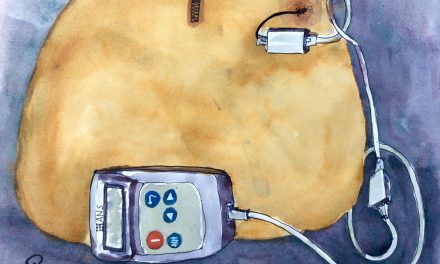
If oral medication does not help and the shoulder bursitis does not resolve on its own, your healthcare professional may recommend a corticosteroid injection to the bursa. While some research demonstrates a significant amount of pain relief for most patients, there is no evidence of long-term pain relief.
Shoulder bursitis exercise
Exercises for shoulder impingement may also likely work for shoulder bursitis because both usually occur together. These include:
Internal and external rotation
This exercise can be done with a cable machine, elastic band, or similar equipment.

(Photos by Penny Goldberg)
Back rows
Any kind of rows would work on all the shoulder muscles as well as the back and abdominal muscles.
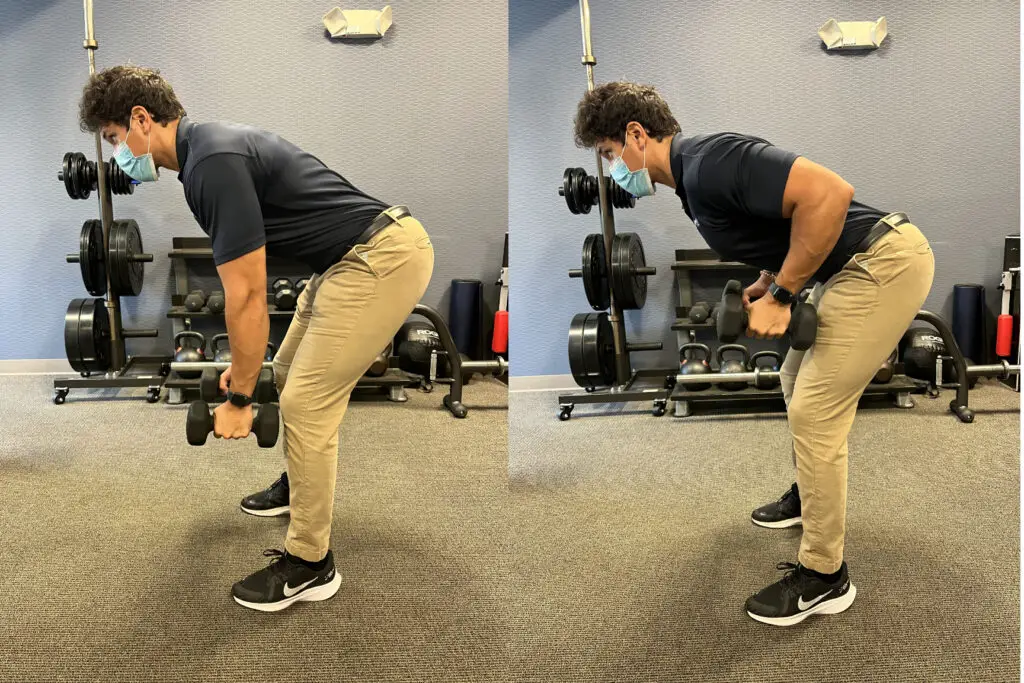
(Photo by Penny Goldberg.)
Shoulder depression
The shoulder depression exercise involves lowering the shoulders downward to engage and strengthen the muscles that stabilize the shoulder blades.
Serratus punches
Scaption
A scaption exercise involves lifting the arms diagonally upwards, typically with the thumbs pointing upwards, to engage the shoulder muscles. You may also do this with pair of dumbbells or an elastic band.
“Shoulder bursitis is also a subacromial impingement [where] the bursa or the rotator cuff tendons can be pinched in the subacromial space,” Dr. Susanna Lin said, who is a physical therapist at Pacific Medical Centers in Seattle, Washington. “I use the same exercises because you’re getting the shoulder to position and move correctly. I usually start with things like pendulums and rows to calm it down, then progress to pain-free strengthening exercises of all the muscles surrounding the shoulder.”
Lin’s exercise suggestions also include:
- Start with lower reps and gradually increase as the patient can tolerate
- Add exercises that doesn’t hurt the patient
While some manual therapists may suggest specific shoulder exercises, current evidence suggests that they are not that better than general exercises, such as jogging and calisthenics.
However, a 2019 Swedish study found that eccentric exercise training—where the movement is emphasized on the lengthening of a muscle under tension—“may provide a small but likely not clinically important reduction in pain” for patients with shoulder impingement. A six- to eight-week rehab program was just as effective as a 12-week program.
“The biggest thing I want to differentiate when treating a shoulder is to determine if it’s a frozen shoulder or something else,” Lin added. “Frozen shoulders will feel different and have a tight end feel. Then I do a ton of stretching, even into pain as long as it feels better/looser as you do more reps or after you’re done.”
Shoulder bursitis surgery
While there’s no evidence that surgery may or may not work for shoulder bursitis, we can examine the research about shoulder impingement, which may translate to shoulder bursitis.
Most physicians recommend surgery for shoulder bursitis if conservative treatments fail. A 2006 systematic review found that arthroscopy shoulder surgery for shoulder impingement is more effective than open acromioplasty with regard to functional limitations and return to work in the short term. However, in the long run, both types of surgeries are “equally effective” in improving function.
The authors warned that most of the 18 studies reviewed were of low quality due to bias, such as lack of blinding of the practitioners in 70% of the trials and lack of mentioning of treatment allocation or whether the patients had more than one treatment. Thus, the conclusion and results are likely provisional, especially for shoulder bursitis since there is a lack of sufficient evidence about it.
More recent evidence suggests that subacromial decompression surgery “provided no important benefit compared with placebo surgery or exercise therapy,” according to a 2020 systematic review.
Massage therapy
Massage therapy likely would not affect shoulder bursitis much and may alleviate symptoms in the short term.
Massage can help relax the tight muscles around the shoulder joint and reduce sensitivity in the nervous system, which can reduce compression and irritation of the inflamed bursa. This may help alleviate pain and improve mobility. However, directly massaging the inflamed bursa itself may likely cause more pain and irritation.
While there are no known protocols or specific massages to treat shoulder bursitis, it’s likely that almost any type of massage that the patient prefers would help, as long as it does not worsen the bursitis, pain, or shoulder function.
If you have symptomatic shoulder bursitis, working with a team of healthcare professionals, and proper self-care may ease the pain and suffering on your road to recovery.
Descending Modulation: Why Massage Therapy Can Help Alleviate Pain
How Massage Therapy Treats Chronic Pain
A native of San Diego for nearly 40 years, Nick Ng is an editor of Massage & Fitness Magazine, an online publication for manual therapists and the public who want to explore the science behind touch, pain, and exercise, and how to apply that in their hands-on practice or daily lives.
An alumni from San Diego State University with a B.A. in Graphic Communications, Nick also completed his massage therapy training at International Professional School of Bodywork in San Diego in 2014.
When he is not writing or reading, you would likely find him weightlifting at the gym, salsa dancing, or exploring new areas to walk and eat around Southern California.