Arthritis refers to different types of joint diseases that are characterized by pain, inflammation, stiffness, swelling, and reduced range of motion. These include:
- Osteoarthritis – Degenerative joint disease caused by cartilage wear and tear
- Rheumatoid arthritis – An autoimmune disorder that targets joint lining
- Psoriatic arthritis – Arthritis associated with the skin condition psoriasis
- Gout – Caused by uric acid crystal buildup in joints
- Ankylosing spondylitis – Inflammation primarily affecting the spine
- Juvenile arthritis – Arthritis in children, including various subtypes
- Reactive arthritis – Triggered by infections in other parts of the body
- Lupus arthritis – Arthritis associated with the autoimmune disease lupus
- Septic arthritis – Infection in a joint leading to inflammation
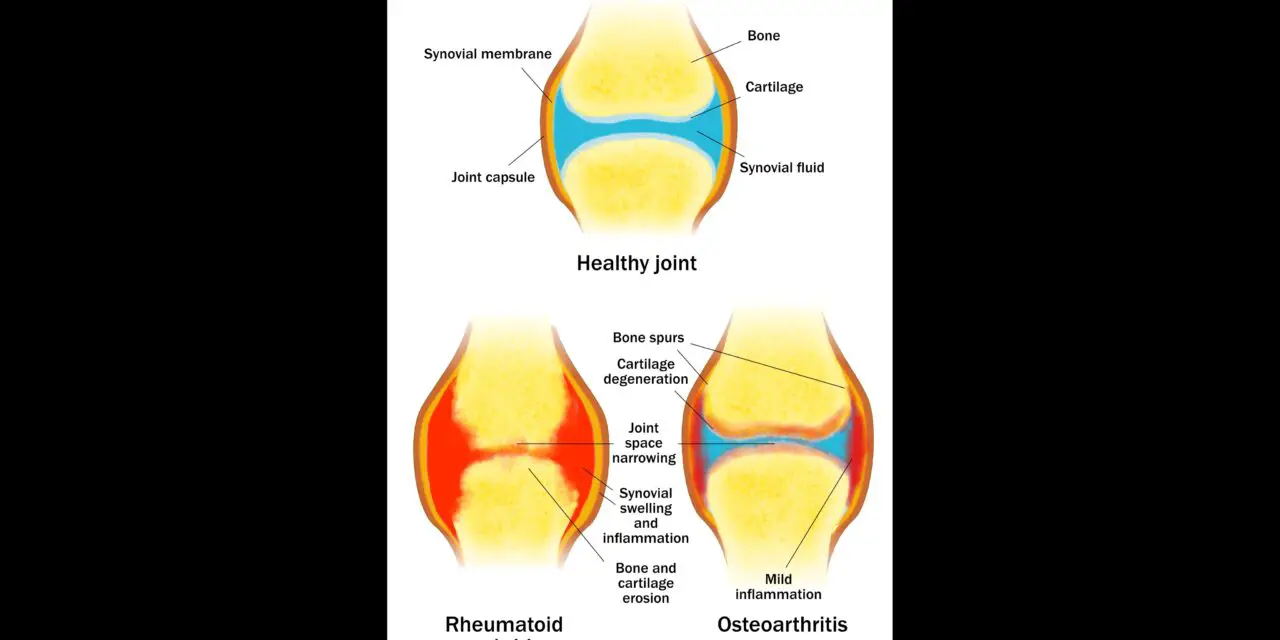
Different types of arthritis require distinct treatments because each type has unique causes, mechanisms, and symptoms. For example, osteoarthritis involves cartilage degeneration and may be managed with physical therapy or joint replacement. However, rheumatoid arthritis is an autoimmune condition often treated with immunosuppressive drugs.
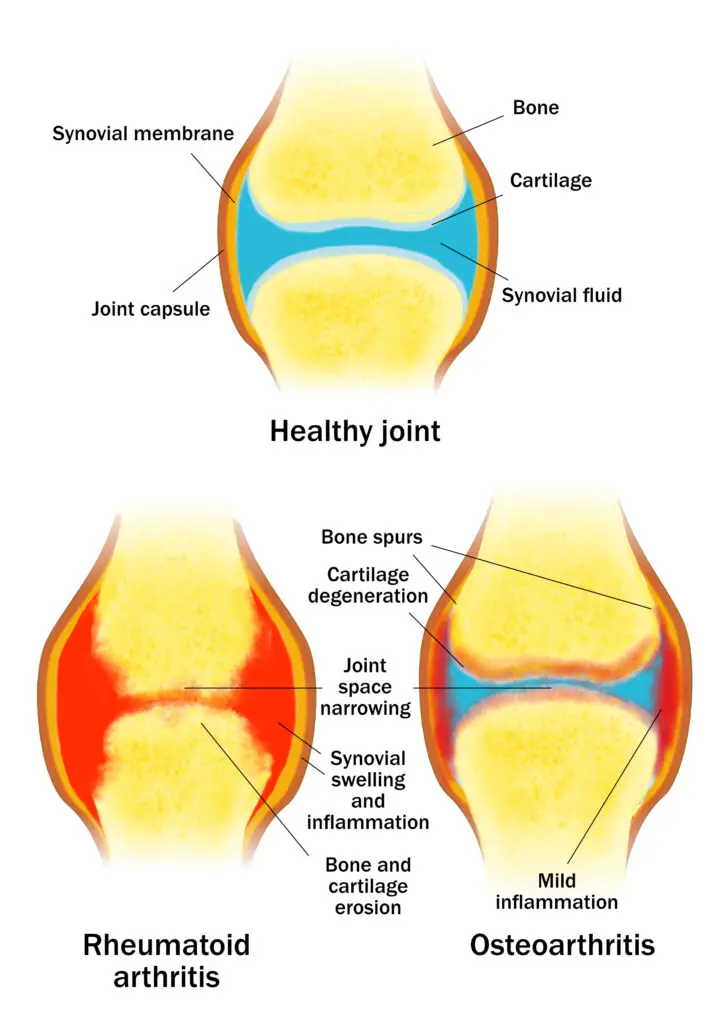
Although different types of arthritis have overlapping symptoms, the primary causes are often different, which requires different frameworks of treatment. (Image by Nick Ng)
Likewise, gout requires medications to reduce uric acid levels, and psoriatic arthritis may involve treatments that target both skin and joint inflammation. Thus, personalized treatments are necessary to address each type’s underlying causes and manage specific symptoms.
Although medicine and surgery are two primary treatments for arthritis, adjunct therapies—such as physical therapy, massage, and exercise—can improve the quality of life.
This review takes a snapshot of the existing evidence of these therapies for arthritis.
Osteoarthritis
Osteoarthritis was thought to be a disease of “wear and tear.” This idea suggested that chronic overuse and poor joint mechanics led to the deterioration of the articular cartilage, resulting in inflammation, stiffness, swelling, and reduced mobility. However, current understanding reveals osteoarthritis as an intricate process involving both inflammatory and metabolic factors, not just biomechanics.
Treatment for osteoarthritis
While there’s no cure for osteoarthritis, there are treatments that can reduce your risk of getting osteoarthritis or delay disease progression.
Weight and body fat reduction
Obesity is a significant risk factor for getting rheumatoid arthritis. In a 2011 randomized-controlled trial, the researchers found that losing 10% of body weight greatly reduced the vertical pressure on knee joints by 11% at the hamstrings.
Another study suggested that women who lost 5 kilograms lowered their risk of painful knee osteoarthritis by 50%.
Exercise
Exercise has been found to help reduce joint pain and improve function for those with knee and/or hip osteoarthritis, based on a 2013 meta-analysis of 60 randomized-controlled trials. This study also suggested interventions that combined strengthening, flexibility, aerobic exercise, and aquatic exercise may be effective; and no type of exercise is significantly better than another.
A 2015 Cochrane review of 55 studies of land-based exercise for knee osteoarthritis found:
- High-quality evidence from 44 trials with 3,537 people showed that exercise significantly reduced pain right after treatment.
- High-quality evidence from 45 studies with 4,607 participants showed that the chance of people dropping out of the exercise group (14%) was similar to those in the control group (15%) with no significant differences.
Also, exercise moderately reduced pain and improved function immediately after the session and slightly improved quality of life.
Bracing
Unloading knee braces may offer some relief from medial and lateral knee osteoarthritis. Knee sleeves that surround the kneecap or applying tape might be beneficial in reducing pain and improving function.
However, a 2015 systematic review of 13 studies found the evidence to be “inconclusive” of bracing for pain, stiffness, function, and quality of life among patients with medial or lateral knee osteoarthritis. The authors also noted that moderate-quality evidence finds a lack of bracing effect on pain, function, and stiffness, while low-quality evidence finds the opposite.
Related: 5 best Donjoy knee braces
Self-management programs
Self-management and educational programs have been shown to have moderate effects in reducing pain and improving function for people with osteoarthritis at four to six months. However, at 12 months, the effects were shown to have smaller effect.
The self-management programs give patients the tools, knowledge, and locus of control of their symptoms. Researchers Dr. Kate Lorig and Dr. Halsted Holmon identified seven factors that self-management programs should have:
- Self-efficacy building
- Self-monitoring
- Goal setting and action planning
- Decision-making
- Problem-solving
- Self-tailoring
- Partnership between the views of patients and health professionals
These programs should also be community-based and close to home so that patients have access to the interventions, they suggested.
Psychological treatments
Because pain is also influenced by psychological, sociological, and environmental factors, psychological treatments may reduce osteoarthritis pain.
Cognitive behavioral therapy (CBT)—a type of psychotherapy using structured sessions to help patients identify and modify negative thinking and behaviors—have shown to help reduce knee osteoarthritis pain when it is combined with exercise, according to a 2021 systematic review of six studies. However, the authors warned that the small number of studies may not be enough to establish a strong association in favor of CBT.
A 2022 systematic review and meta-analysis of 15 trials show a “promising alternative or complementary intervention” in reducing pain, insomnia, and depression related to osteoarthritis during the follow-up period. However, there was no significant improvement in sleep efficiency, fatigue, or physical function.
Rheumatoid arthritis
Rheumatoid arthritis is a disease that affects the whole body, including joints, heart, kidneys, lungs, digestive system, skin, eyes and the nervous system. It happens when the immune system mistakenly attacks healthy parts of the body, causing long-lasting inflammation that can damage joints and other organs.
Rheumatoid arthritis is a form of undifferentiated connective tissue disease, a broad term used for conditions that show features of multiple connective tissue diseases but don’t fully match the criteria for any single specific disease. The overlapping symptoms make it challenging for doctors to accurately diagnose and safely treat these conditions.
Treatment for rheumatoid arthritis
Besides standard medications, such as DMARDS (disease-modifying antirheumatic drugs) that target specific molecules that cause inflammation, there are several conservative options that are used to treat rheumatoid arthritis with the medications.
Exercise
Exercise has been shown to reduce the symptoms of rheumatoid arthritis. A 2023 review highlighted that exercise may:
- Temporarily boost leukocyte counts and alter immune functions, which might help reduce the severity of the disease and improve the body’s maladaptive autoimmune response.
- Decrease inflammation and disease activity, but the biological mechanism is unclear
- Reduce the activities of matrix metalloproteinase, which are a family of enzymes that breaks down proteins in the extracellular matrix, the spaces between cells.
A 2020 study of 10 systematic reviews of exercise and rheumatoid arthritis found that most types of exercise have positive effects of reducing symptoms while improving physical fitness.
For example, the researcher found that strength training had a “positive effect” on pain, yet it does not improve aerobic capacity or physical function. Aerobic exercise may decrease pain if exercise is maintained for three months; however, there were no additional benefits at six months.
Occupational therapy and physical therapy
Occupational therapists work with rheumatoid arthritis patients to develop personalized strategies for joint protection, energy conservation, and task modification, enabling them to perform daily activities more efficiently and with less discomfort. They may recommend and teach you how to use assistive devices or adaptive equipment to make your work easier.
Physical therapists can help rheumatoid arthritis patients develop personalized exercise plans that match their abilities and fitness levels. These plans include flexibility, strength, and cardiovascular exercises without exacerbating symptoms or causing acute flare-ups.
Massage therapy
Massage therapy may reduce the pain associated with rheumatoid arthritis. For example, a 2021 study on massage effects of patients with rheumatoid arthritis found that those who receive regular Swedish massages for eight weeks had less pain and less reliance on pain medication than the control group who had routine care.
Since massage research about arthritis is limited and tends to have high risks of bias, any claims about what massage can do for arthritis should be considered cautiously.
Psoriatic arthritis
Psoriatic arthritis is characterized by inflamed, swollen, and painful joints, often occurring in people with psoriasis, a skin condition causing red, scaly patches. It can affect various parts of the body including fingers, toes, spine, and other joints.
A key distinguishing feature of psoriatic arthritis is the presence of dactylitis, or “sausage digits,” where entire fingers or toes become swollen. Psoriatic arthritis can also cause enthesitis, an inflammation at where tendons and ligaments connect to bones, which is not typically seen in other forms of arthritis.
Treatment for psoriatic arthritis
With prescribed anti-inflammatory medications, there are several conservative options that are used to treat psoriatic arthritis.
Exercise
A 2021 systematic review of 13 studies found that exercise can reduce the symptoms of psoriatic arthritis while improving cardiovascular health and muscle strength. Interestingly, the researchers did not find evidence that exercise can worsen the tendon and ligament attachments.
Physical therapy
While the evidence and data for physical therapy and psoriatic arthritis is scarce, physical therapists can guide patients with a customized exercise program and keep track of their progress. Also, fat loss can reduce psoriatic arthritis symptoms as well as metabolic issues.
There are no standard guidelines for exercise dosage.
Gout
Gout is the sudden, severe episodes of pain and swelling in the joints, mostly at the big toe, caused by the buildup of uric acid crystals in the body. It’s often accompanied by various comorbidities, including cardiovascular disease, chronic kidney disease, obesity, and other conditions.
Treatment for gout
Besides NSAIDS, corticosteroids, interleukin-1β inhibitors, and other pharmacological interventions, physical therapy, exercise, and massage could manage flare ups and other symptoms from gout.
Physical therapy and exercise
Physical therapy and exercise could reduce uric acid levels in the blood, which may lead to fewer acute gout flares, according to a 2021 systematic review of 10 studies. One of these studies reported that physically active men with gout had at least 12 times fewer gout flares per year and nearly three times less likely to experience pain after a four-week treatment period compared to physically inactive men.
However, exercise and physical therapy wouldn’t work well if diet, excess alcohol intake, stress, and smoking habits are not addressed.
Massage
There’s no research that specifically targets massage and gouty arthritis. However, existing research on other types of arthritis may yield similar results in reducing acute pain. Massage therapists should take a detailed medical and lifestyle intake prior to treatment first-time patients while addressing the unique experiences of each patient.
Heat and cold therapy
A 2022 study reported that patients with gout who had undergone alternating warm and cold treatments had improved sleep quality and lower serum uric acid levels than those who did not receive such treatment.
Based on another study on warm footbaths for cancer patients, perhaps the physiological and psychological benefits of having touch and care can carry over to patients with gout as well as other types of maladies.
Ankylosing spondylitis
Ankylosing spondylitis is a chronic inflammatory disease that primarily affects the spine, causing pain and stiffness, particularly in the lower back. It can lead to the fusion of vertebrae over time. This condition often begins in young adults and can also involve other joints and areas where tendons attach to bones, resulting in extra symptoms like fatigue and eye inflammation.
Treatment for ankylosing spondylitis
While NSAIDs and TNF-alpha inhibitors are the main drugs for treatment, several non-pharmacological treatments may help in reducing ankylosing spondylitis symptoms.
Physical therapy and exercise
A 2022 study of 12 trials compared physical therapy with usual care and home-based exercise programs among a total of 629 patients with ankylosing spondylitis. The study found that physical therapy is “more effective” than usual care in reducing disease activity and pain and improving patients’ daily functions. However, there were no significant differences between physical therapy and home-based exercise programs.
While exercise has been shown to reduce the symptoms of ankylosing spondylitis, a 2016 study reported that there hasn’t been specific prescriptions on the exercise dosage, and no type of exercise is better than another.
The researchers suggested that clinicians should stick with the FITT principle (frequency, intensity, time, type) to modify the exercise program for each patient. Other factors that influence exercise modification include pain, fatigue, disease activity, cardiorespirator issues, osteoporosis, and balance impairment.
Massage
One small 2017 study of 27 men found that there was no difference in disease activity and flexibility test outcomes between the deep tissue massage and therapeutic massage. However, the researchers found that the deep tissue group reported lower low back pain than the therapeutic group.
Due to the small sample size, the researchers wrote that the results “do not allow for final conclusion” about the role of massage therapy for ankylosing spondylitis.
Another study reported a patient who had tui na massage at his neck was admitted to an emergency room with quadriplegia and labored breathing. He died seven days after admission due to respiratory failure and cardiovascular dysfunction. The researchers reported that excessive compressive forces that are commonly used in tui na may have fractured the neck.
Juvenile arthritis
Juvenile arthritis refers to arthritis that affects children and teens, which encompasses a group of autoimmune conditions that lead to joint inflammation in those under age 16. Unlike adult forms of arthritis, juvenile arthritis may go into remission and is often outgrown by children as they mature.
Juvenile arthritis symptoms typically last for at least six weeks and can vary widely among affected children. For instance, oligoarticular juvenile arthritis affects four or fewer joints and is the most common form, while polyarticular juvenile arthritis involves five or more joints and can resemble adult rheumatoid arthritis.
Treatment for juvenile arthritis
Besides NSAIDs, DMARDs, and other medications that are typically prescribed for arthritis, physical therapy, exercise, and other non-pharmacological treatments are available for those with juvenile arthritis.
Physical therapy and exercise
One 2023 systematic review of 18 trials found that patients with juvenile arthritis who underwent physical therapy as part of their treatment had improvements in quality of life, pain, physical functions, gait, and aerobic conditioning compared to those who didn’t receive physical therapy.
Another systematic review on exercise therapy for juvenile arthritis reported the mixed methodologies of the experiments and the lack of high-quality evidence “limited the ability to provide conclusive, generalizing evidence for the efficacy of exercise therapy and to provide specific recommendations for clinical practice.”
Septic arthritis
Septic arthritis is typically caused by bacteria that spread through the bloodstream from one body part to another or enter directly through an injury or surgical site. It usually affects one large joint, such as the knee or hip, causing sudden severe pain, swelling, and limited mobility.
Treatment for septic arthritis
Depending on the diagnosis and type of septic arthritis, a physician would do a joint drainage and administer antibiotic therapy. They may use needle aspiration for accessible joints, arthroscopy for more precise drainage, or open surgery for deeper joints like the hip.
The choice of antibiotics depends on which organism causes the disease, which is identified through synovial fluid analysis. Treatment duration is usually at least two weeks for small joints, but more commonly extends to four to six weeks to ensure complete eradication of the infection.
Physical therapy and exercise
While medicine and surgery has lowered the mortality rate in people with septic arthritis, rehabilitation—including physical therapy—remains “poorly codified and is often delayed,” according to a group of researchers from Université Clermont Auvergne in France.
They wrote that studies on animals have shown that controlled physical stress can help strengthen cartilage and reduce inflammation by affecting certain chemicals in the body. In a model of septic arthritis, continuous passive movement was found to lower the risk of bone spurs, tissue growth in joints, and cartilage damage. However, these effects haven’t been studied much in humans. While early movement might improve recovery, clear guidelines for early rehabilitation are still lacking.
“Despite the lack of existing studies in humans in the literature, early rehabilitation management of patients with septic knee arthritis in native joints should improve functional prognosis and help reduce oedema and pain,” the researchers concluded.
An Indian case study of a 58-year-old man with septic arthritis in his knee found that a customized physical therapy program that included strengthening, range of motion exercises, and endurance training is “highly effective at enhancing the patient’s functional independence and quality of life.”
Lupus arthritis
Lupus arthritis is a common symptom of lupus, a disease where the body’s immune system attacks its own tissues. In lupus arthritis, the joints become inflamed, causing pain, swelling, and stiffness. This typically happens in the small joints of the hands, wrists, and feet, and it often affects both sides of the body equally.
Unlike some other types of arthritis, lupus arthritis usually doesn’t permanently damage the joints. However, in rare cases, it can lead to joint deformities over time. People with lupus arthritis might find it hard to do everyday tasks due to joint pain and stiffness, especially in the morning or after resting for a while.
Lupus arthritis is sometimes called systemic lupus erythematosus (SLE).
Treatment for lupus arthritis
Besides medications, such as NSAIDS and hydroxychloroquine for mild cases of lupus and corticosteroids for more severe cases, there are several non-pharmacological treatments that serve as adjuncts to improve function and reduce pain.
Physical therapy and exercise
According to an international task force in 2023, the amount and type of exercise recommended for someone with lupus arthritis would depend on the type of symptoms, diagnosis, exercise preference and tolerance, and contraindications provided by a physician.
For cardiovascular health, the task force recommends a gradual progression of aerobic exercise that targets 40%–75% of the heart rate reserve, which is the difference between a person’s maximum heart rate and resting heart rate.
Strength training should be performed for 1 to 3 sets per exercise for 8 to 12 reps with 1 to 3 minutes of rest between sets. Weekly frequency should be three to five days a week.
Despite the recommendations, a 2023 systematic review of 13 studies found that the addition of exercise to usual pharmacological care “may have little to no effect on fatigue, functional capacity, and disease activity.”
“We are uncertain of the potential for harm from structured exercise, because of the limited number of studies reporting adverse events. We are unable to distinguish the best dosage of exercise, including frequency, intensity, type, or its mode of delivery,” the researchers reported.
Nick Ng is the editor of Massage & Fitness Magazine and the managing editor for My Neighborhood News Network.
An alumni from San Diego State University with a bachelor’s in graphic communications, Nick also completed his massage therapy training at International Professional School of Bodywork in San Diego in 2014. In 2021, he earned an associate degree in journalism at Palomar College.
When he gets a chance, he enjoys weightlifting at the gym, salsa dancing, and exploring new areas in the Puget Sound area in Washington state.