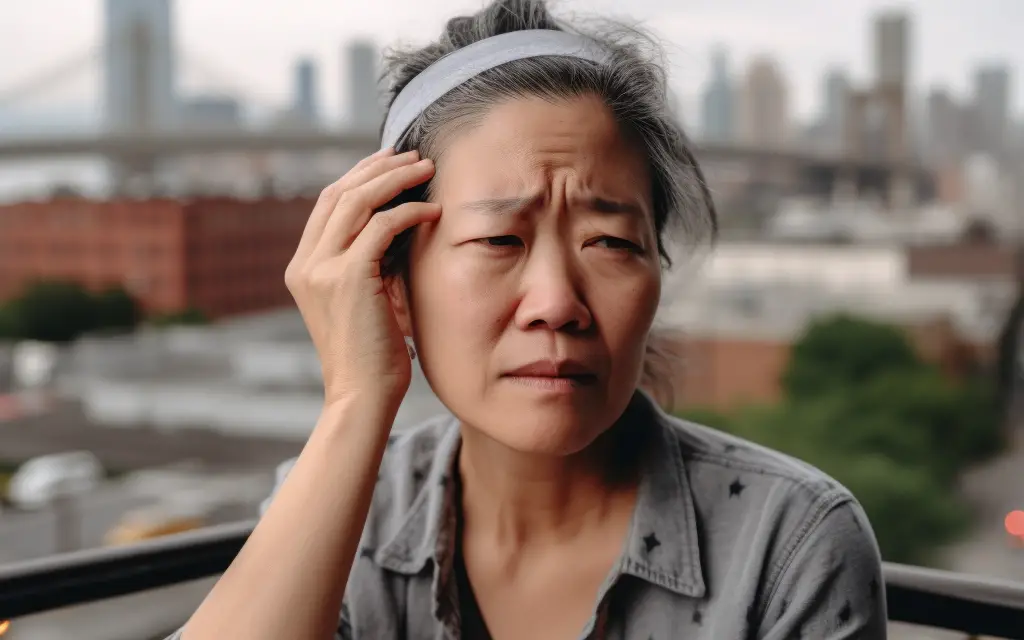
Migraine attacks are a common symptom of Ehlers-Danlos syndrome (EDS) that a majority of people with this condition experience. Current evidence suggests that it’s primarily caused by connective tissue abnormalities, such as weak collagen fibers, that are influenced by genetic factors. This can cause blood vessels in the brain to be more susceptible to inflammation and damage, which can trigger a migraine.
On top of that, people with EDS may also have neck, jaw, and/or back pain. While no one can pinpoint what causes it, some researchers hypothesize that instability of the spine and the stress that accompanies pain create a vicious pain cycle.
What is a migraine?
A migraine is a type of headache that runs in families and is caused by changes in how your brain processes sensory information, including touch and pain. They have a variety of symptoms, but the most common and recognizable one is a headache.
A typical migraine attack among those with EDS can last between 4 to 72 hours (three days) and consists of four phases that overlap each other:
- Premonitory phase: Symptoms with no pain appear within hours or days before the headache sets in. These symptoms may include excessive yawning, mood changes, difficulty in concentration, neck stiffness, fatigue, thirst, and frequent urination.
- Aura: In this phase, symptoms include flashing lights like a kaleidoscope, tingling in the hands and feet, and narrowed or tunnel vision. It usually starts with distorted vision followed by sensory changes in the skin and speech, but there are cases where the order of symptoms are reversed. However, people with EDS typically do not experience an aura during a migraine attack.
- Headache: Symptoms include pulsating pain on one side of the head, sensitivity to light, sound, and smell, vertigo, nausea, vomiting, and discomfort or pain from light touch.
- Postdrome: Sometimes called a “migraine hangover,” the postdrome phase is the least studied of all the phases. While the symptoms are similar to the premonitory phase, some patients have reported constipation, excessive flatulence, fluid retention, and insomnia. This phase tends to last longer if you have higher pain intensity.
How does EDS cause a migraine?
While no one really knows if EDS is a major cause of a migraine or vice versa, current scientific evidence points to a few clues of some major risk factors.
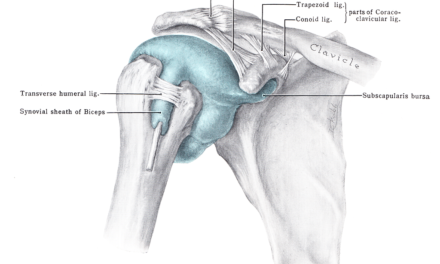
Lax ligaments
Ligamentous laxity, or loose ligaments, is a main symptom of hypermobile Ehlers-Danlos syndrome. Migraine, with or without aura, is often experienced by patients with this condition. It has been hypothesized that the craniocervical instability that results from the loose ligaments that support the C1 and C2 of the cervical spine, which can cause the headache.
The 5th cranial nerve—the trigeminal nerve—is the main sensory component of pain in the head and face. The primary nucleus for this nerve is housed in the brainstem and upper cervical spine. This is called the trigemino-cervical complex and is thought to be the main physiological driver behind headaches caused by irritation to the upper cervical spine.
Intracranial Pressure
Idiopathic intracranial hypertension (IIH) may also be a cause of migraine attacks if you have hypermobile EDS. There are multiple hypotheses describing how this might happen. One thought is that too much production of cerebrospinal fluid causes the increased pressure, which leads to the headache. Another suggests that the veins responsible for draining blood from the brain can be obstructed causing increased pressure in the venous sinus.
Pinched nerves
Instability of the cervical spine, particularly at the atlas, may also lead to pinched nerves near the joints in the neck that move too much. An injury to these nerves would likely be accompanied by a protective muscle spasm. Pain from the nerve injury and decreased blood flow to the brain from the tight neck muscles is the perfect combination to create a headache or migraine.
Biomarkers
Research since the early 1990s found a few significant biomarkers (biological molecules in the bloodstream) that may cause a migraine attack. One of these is called CGRP (calcitonin gene-related peptide), which is a protein that is produced in the cell bodies of neurons both in the spinal cord and peripheral nerves. CGRP plays a role in dilation of blood vessels and a regulator of nociception, where 13 out of 20 studies found a positive association between the biomarker and migraine symptoms. Numerous studies since 2002 found that between 40% to 60% of test subjects will get a migraine when they are infused with CGRP.
And because of the lax tissues in people with EDS, it’s possible that such condition can make blood vessels in the dura mater more permeable, which makes it easier for CGRP and other biomarkers to travel through.
Some researchers points to three potential sites where CGRP can trigger a migraine:
- The widening of blood vessels through the action of two molecules called cyclic adenosine monophosphate (cAMP) and cyclic guanosine monophosphate (cGMP);
- The stimulation of sensory nerves in the trigeminal ganglion and nerve pathways;
- Changes in how the brain “perceives” nociception and external stimuli
Other biomarkers that can also trigger a migraine attack include:
- pituitary adenylate cyclase-activating polypeptide (PACAP)
- adenosine triphosphate-sensitive potassium (KATP) channel
- large conductance calcium-activated potassium (BKCa) channel
By identifying these biomarkers, researcher can create medications that target their receptors which prevents the chain reaction that cause a migraine.
When should you see a doctor?
As a general rule, it’s always okay to see your physician about pain. That said, you should seek care if you have been diagnosed with EDS and can no longer manage your symptoms with your usual medications. You should see your doctor before increasing doses or changing medications.
You should also consult with your physician if your EDS-related migraine attacks are negatively affecting your quality of life or ability to perform every activities. You may want to see emergency care if you have a migraine accompanied by changes in neurological function (weakness, numbness), confusion, double vision, difficulty speaking, or neck stiffness. A headache that doesn’t feel like an ordinary headache is also cause for a visit to a healthcare provider.
Migraine attacks related to EDS can be caused by serious systemic conditions. You should be sure to ask your physician to rule out a cerebrospinal fluid leak and how you can best manage the instability associated with your condition. A referral to a physical or occupational therapist may be warranted to help you learn to manage your everyday tasks with this condition.
The warning signs of a migraine can be as variable as the condition. You may be irritable, have difficulty sleeping, or feel anxious. Cravings, throbbing pain in the head, neck or eye pain, yawning, and constipation may also precede a migraine.
What works for treating migraines and EDS?
Though the research is sparse, there seems to be a connection between hypermobility disorders, cervical spine instability, and headaches. As such, there are several options for treatment that may work alone or in combination to help manage your symptoms.
A large retrospective study of patients with hypermobility disorders found that the head and neck symptoms responded well to targeted therapy for the cervical spine.This therapy included epidural injections, retro-laminar cervical blocks, and Botox injections. Researchers concluded that the positive responses to these therapies suggests that degenerative conditions of the spine may play a role in the headaches that patients with hypermobility experience.
How can massage therapy help with migraines and EDS?
The benefits of massage on a variety of conditions have been well-established. Patients with conditions such as juvenile rheumatoid arthritis, fibromyalgia, multiple sclerosis, disordered eating, breast cancer, chronic fatigue, and diabetes have all been helped by massage.
The psychological impact of EDS is well established. A 2008 study out of Sweden found that nearly 75% of participants self-reported anxiety and 22% reported depression. Research has long shown massage to be an effective modality for reducing both. Single sessions of massage therapist can improve momentary emotional experiences such as nervousness, tension and worry. Multiple sessions performed over days to weeks can have even more impressive effects in the ability to decrease trait anxiety or the tendency to feel anxious in most situations.
Generally speaking, when you are stressed your body releases stress hormones that lead to muscle tension and pain. The overall relaxation effects of massage therapy can decrease muscle tension and anxiety as well as decrease pain.
Massage can also play a role in your body’s release of serotonin, which is the neurotransmitter connected to feelings of well-being and happiness. The release of serotonin also decreases cortisol—the stress hormone which can create muscle tension and pain. Massage also influences the release of endorphins (also known as endogenous opioids or natural painkillers) which can decrease stress, reduce pain levels, and improve stress levels.
Massage therapy may be a helpful adjunct in the management of EDS when it comes to pain control. The frequent joint dislocations that accompany hypermobility often leaves patients in constant, chronic pain. Massage therapy can help these patients through pain reduction, decreased muscle tightness, and overall relief of stress and anxiety.
Notably, a review of the research on the current treatments for EDS found that massage was second to opioids for effectiveness of relief for acute and chronic pain.
Resources for migraines and EDS
EDS is a life-changing diagnosis but it does not have to be debilitating. Local and online support groups are waiting to support you and help you manage the complexities of your diagnosis. To find a local support group, patientrising.org is a great place to start.
Chronic Pain Partners is another amazing resource. Through their campaign to raise awareness of all things EDS, this non-profit will not only offer you local support groups, but it will also show you how to start your own if one is not available in your area!
Chronic Pain Partners also has more than 50 webinars and educational recordings from EDS experts available at the touch of a button. If in-person isn’t available or isn’t for you, the Ehlers-Danlos Society offers virtual support groups as well. Whether you choose in-person or virtual support, the time is now to connect with others who are thriving through their EDS diagnosis!