Six years after releasing their initial recommendations on prescribing opioids for chronic pain, the Centers for Disease Control (CDC) updated the federal guidelines last February, emphasizing on trying other treatments in the management of acute and chronic pain before prescribing opioid medications.
The suggested non-opioid treatment options are both pharmaceutical and non-pharmaceutical, such as gabapentin and over-the-counter pain relievers like ibuprofen, physical therapy, acupuncture, and massage therapy , are among the list of things to try when it comes to pain management with the lowest effective dose of the opioids.
Massage therapy may decrease stress, depression, and anxiety, reduce muscle pain and soreness, and lower blood pressure. These benefits position massage therapists among first-line providers to help these patients manage their pain.
How does massage therapy help with pain control?
Pain is the reason most people seek care from health care providers. It’s a unique, individual experience and should not be treated with a one-size-fits-all approach. Several studies show massage therapy is an effective treatment for pain and this is reflected in the revised CDC guidelines with the inclusion of massage therapy as a viable option for treating pain.
A 2016 systematic review and meta-analysis in Pain Medicine looked at 67 studies and found clear evidence to support the use of massage therapy for pain management. When compared to sham or active interventions, massage therapy also decreased anxiety and improved health related quality of life.
The underlying reason that massage therapy relieves pain is difficult to narrow down to a single mechanism of action. Just as pain is a unique experience, so are massage and physical touch.
Several studies show an increase in parasympathetic nervous system (rest and digest) activity is at least somewhat responsible for the positive effects of massage. The parasympathetic nervous system is well known for its role in calming pain sensitivity and helping to create general relaxation when pain doesn’t need to be felt.
The mechanism of pain relief from massage isn’t completely clear, however, one path may be through decreasing stress and thereby cortisol levels in your body. When pain is the cause of stress, cortisol not only intensifies the pain but also creates a fear-based memory.

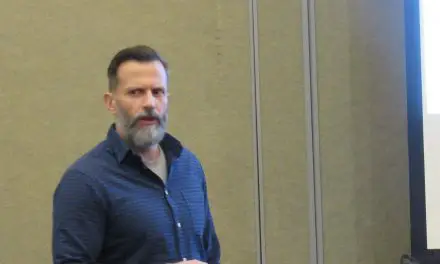
Lisa Flores, LMT, gives Eric Ouellet a chair massage during the 2020 San Diego Pain Summit. (Photo by Nick Ng)
In a 2014 study that investigated the use of therapeutic massage for chronic neck pain, 220 patients with chronic neck pain were grouped by various dosages of massage therapy: four weeks total consistenting of either 30-minute visits two or three times a week or 60-minute visits one, two, or three times a week. Researchers found that longer massages provided more pain relief than no massage, fewer sessions, or shorter sessions.
Massage may also play a role in improving immune system function which leads to decreased pain. Research published in the International Journal of Cancer found that both stress and surgery reduced resistance to tumor development in rats by decreasing the production of NK, or natural killer cells.
These cells are known for detecting and controlling early signs of cancer as well as killing virally infected cells. NK cells also enhance the immune response by secreting cytokines that act on other players in the immune system (macrophages and dendritic cells). To say we need NK cells is an understatement.
Massage therapy can help NK cells survive and thrive. Researchers employed massage therapy in a group of 34 women with Stage 1 or 2 breast cancer who had undergone surgery.
Those in the experimental group recieved 30-minutes of massage three times a week for five weeks. Patients reported the early effects of massage included decreased anxiety, depression, and anger. In the long term, these patients continued to experience lower levels of depression and hostility along with increased dopamine, serotonin, NK cells, and lymphocytes.
Similar results were found in patients with HIV after receiving daily massage for a month. In these patients, decreased anxiety and increased relaxation were correlated with increases in NK cells. These findings suggest the effects of massage can increase cytotoxic capacity, which has implications for patients with illnesses beyond HIV and cancer.
So what does massage therapy do?
Massage therapy can do more than just relieve pain. A study in Complementary Therapies in Clinical Practice found that therapeutic massage was only one piece of the puzzle for participants. After having weekly massages and being taught to perform daily self-massage, these patients also reported improved sleep as well as decreased anxiety and depression.
In 2017, the Department of Health and Human Services suggested that healthcare organizations help fight the opioid crisis by finding alternative, evidenced-based methods for pain control.
The nurses on the medical-surgical unit of Meritus Medical Center in Hagerstown, Maryland, an area that saw an increase in opioid-related deaths over a short period in 2019, set out to do their part. Massage therapy was offered as weekly 15-minute sessions.
At the end of the four-week study, patients reported a significant reduction in pain intensity scores, going from nearly a 6 (out of 10) to slightly below a 3. Patients reported not just improvement in pain but also emotional well-being, relaxation, and sleep. There were also two noteworthy cases of patients who had improved oxygenation and lung function following massage therapy.
A similar small study was performed with children receiving palliative care for cancer over a four- to six-week period. The children received hour-long massages once a week. Pain and worry ratings were recorded before and after treatment sessions.
The children reported significant decreases in pain after two sessions and less worrying after a single session of massage therapy. These improvements did not persist through follow-up, suggesting that massage therapy may lead to immediate decreases in pain and worry in children receiving palliative care for cancer but may not be an effective long-term solution.
The National Survey on Drug Use and Health reports on why adults misuse prescription drugs. When specifically asked about misuse of pain relievers, nearly 20% of respondents reported the following reasons: to relax or relieve tension, help with sleep, or to help with emotional well-being.
A 2004 meta-analysis of massage therapy research found that a single massage therapy session can reduce state anxiety. State anxiety encompasses the transient emotional experiences of worry, tension, and apprehension. When multiple sessions of massage therapy are performed over weeks to days, trait anxiety or the normal tendency to experience anxiety can be significantly reduced.
Do pain management systems do massage therapy?
While many cultures worldwide have used massage therapy for pain relief for thousands of years, massage therapy (particularly Swedish massage) was more widely accepted in the U.S. and Canada during the 1800s and evolved into an integral part of health and wellness today.
Massage therapists can be found working in hospitals, ambulatory clinics, hospice care, and private practice. Massage has been embraced by physicians, chiropractors, physical therapists, and other health care professionals as a component of an overall treatment program. That said, the U.S. healthcare system doesn’t make it easy to access massage services.
Despite mounting evidence of its efficacy, insurance companies have been less welcoming. Most American health care reimbursement follows the standards set by the Centers for Medicare and Medicaid Services (CMS).
Strangely, CMS will pay for massage therapy—just not when it’s provided by a massage therapist as this is classified as an alternative treatment.
Massage therapy can provide temporary pain relief, but whether it’s cost effective would depend on many social and economic factors. (Photo by Tima Miroshnichenko)
Although this is bad news for patients with federally-funded insurance, such as Tricare, Medicare, or Medicaid, there are private insurers who pay for massage therapy provided by a massage therapist. It may be difficult to find massage therapists who bill insurance but you can see the massage therapist of their choice, pay for services, and then submit the bills to your insurer for reimbursement as long as the insurer’s requirements are met.
Over the past several years, massage therapists in Canada have started to emerge as integral members of the care team. What began in private spas has spread to private health centers and even hospitals. The role of the massage therapist in the hospital setting was examined in a 2015 study in BMC Complementary Medicine and Therapies.
Researchers found that massage therapists in the hospital setting were still few and far between but could be found in four provinces and in hospitals of varying size, type, and patient-population focus.
The primary term used to describe the role of hospital-based massage therapists was health care provider. As such, the therapists reported they were expected to be subject matter experts while performing assessment and treatment of their patients. They also noted a working knowledge of the patient’s condition including related signs and symptoms was expected.
While it’s great to see the strides massage therapists have made over the past several years, it’s hard to explain why massage therapy still struggles with acceptance in the mainstream medical community.
Further insight: [Could U.S. Masage Therapy Be Part of Healthcare Like Canada?]
Is massage therapy really cost effective?
Because the coverage of massage therapy varies so much by insurance payer, it’s tough to determine widespread cost effectiveness. What we know for sure is that massage therapy is almost never as inexpensive as prescriptions when covered by insurance.
“Until you can give me a policy by which physical therapy, occupational therapy, massage therapy, acupuncture, biofeedback and behavioral health are as cheap as a five-dollar prescription for [an opioid] each month, I’m going to have problems,”said Dr. Rachel Franklin, who is the Physician Executive for Community Health and Primary Care for OU Health.
This sentiment is echoed in the Department of Health and Human Services inter-agency task force report on Pain Management Best Practices. The report identifies improved payment policies, education of medical professionals, and more pain management specialists as a few ways to increase access to complementary and integrative health approaches including massage.
The agencies specifically noted that improved education of patients and providers in terms of guidance and indication for use can help decrease the reliance on opioids.
A 2020 New Zealand study on the cost-effectiveness of interventions for knee osteoarthritis used a computer simulation model to determine if treatments were financially sound.
The model didn’t find massage therapy to be cost-effective regardless of the income level of the patient. One of the reasons is that the uncertainty of lifetime treatment effectiveness is unknown.
In osteoarthritis, the condition is irreversible so the need for massage could last anywhere from weeks to decades, which is similar to what might be predicted for patients with chronic pain.
Finding ways to access massage therapy for those who simply cannot afford it can be tricky. While the insurance plans provided by the Affordable Care Act don’t cover massage therapy as a stand-alone service, they often have low-cost access to physical therapy.
Although the training is different, physical therapists are also well-versed in physical touch, often referred to as manual therapy, and can provide massage that’s covered by insurance.
For those who absolutely want to see a massage therapist, there’s good news. Samantha Ream, a licensed massage therapist and Director of the massage therapy program at ReQuest Physical Therapy in Gainesville, Fla., suggests checking for nearby massage schools and even on social media.

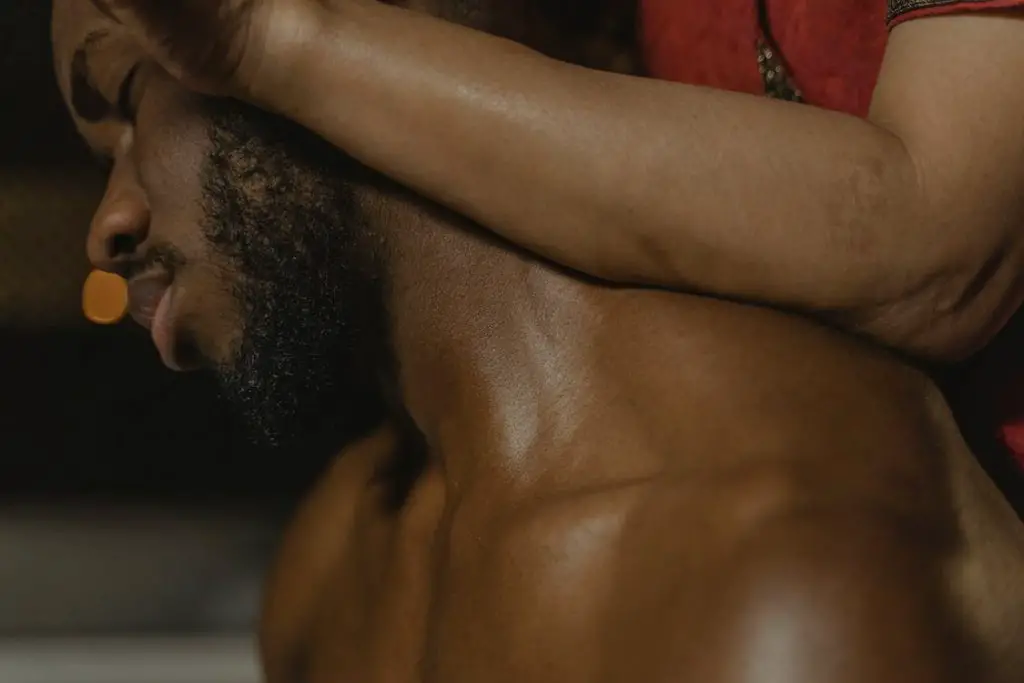
Students at Pacific Center for Awareness and Bodywork in Kauai practices massage therapy. (Photo courtesy of Mark Olson.)
“If there is a massage school nearby, you may be able to access free or low-cost services provided by the students,” Ream said. “There may also be new grads who are working on getting hours toward their certification that need to get their hands-on hours that post in local Facebook groups. [Also], massage therapists love to barter so if there is a skill you can trade for their work, offer it!”
Producing high quality studies on the effectiveness of massage therapy across multiple conditions is key to getting insurance reimbursement. Until this is done, it’s unlikely that massage therapy will be considered a cost-effective treatment for pain or anything else.
What types of massage are best for pain relief?
There are many types of massage that can provide pain relief, and because touch is a subjective experience, the “best” type is the one that works for you. It can be feather-light touch (lymphatic massage), sustained pressure (e.g. deep tissue massage), trigger point therapy, Thai, lomi lomi, or any combination of techniques.
Current research indicates that affective touch of most kinds can alleviate pain. That said, there seems to be other contextual factors—other than massage techniques—that can influence your experience with massage therapy. In fact, expectations seem to play a larger role in the contextual effects of alternative therapies than mainstream medicine.
In a 2017 report “Placebo Mechanisms of Manual Therapy: A Sheep In Wolf’s Clothing,” researchers Bialosky and Bishop highlighted the role of contextual factors when using manual therapy. Therapists who employ manual therapy techniques typically do so with enthusiasm.
These therapists tend to introduce the treatment and explain expected procedures and their benefits with an excitement beyond that of other interventions. Framing the effects of the treatment in a positive light can potentially influence how the patient perceives said treatment by either altering or reinforcing preconceived notions.
This isn’t news to massage therapists. A 2010 study in Complementary Therapies in Medicine looked at the attributes that are most valued by patients who have regular health-related massage therapy. This qualitative study used multiple phone focus groups to gather data.
They found six important elements of the massage encounter: time for care, personal attention, engaging and competent therapists, trust partnership, holism and empowerment, effective touch and enhancing relaxation.
Comfort, contact, connection, and caring were modulators that played a role in creating trust and relaxation to facilitate the effectiveness of the massage.
If you’ve ever had a massage, you likely know this to be mostly true: a quiet room filled with calm, muted colors, warm temperature, and softs linens. The therapist likely spoke softly as they welcomed you. Even if you don’t notice these things, they all influence the perception of the massage experience.
Ream suggests that you try out multiple massage therapists to determine who best suits your needs. “Massage is an incredible tool to reduce pain and improve both physical and mental health when it is done well,” she said. “Massage with the right therapist is a safe place to receive therapeutic touch, quiet your mind, and reconnect with your body.”
Further insight: [Why Massage Therapists Should Understand How Pain Works]

Penny Goldberg, DPT, ATC
Penny Goldberg, DPT, ATC earned her doctorate in Physical Therapy from the University of Saint Augustine and completed a credentialed sports residency at the University of Florida. She is a Board Certified Clinical Specialist in Sports Physical Therapy.
Penny holds a B.S. in Kinesiology and a M.A. in Physical Education from San Diego State University. She has served as an Athletic Trainer at USD, CSUN, and Butler University.
She has presented on Kinesiophobia and differential diagnosis in complicated cases. Penny has published on returning to sports after ACL reconstruction and fear of movement and re-injury.
Outside of the clinic, Penny enjoys traveling, good cooking with great wine, concerts, working out and playing with her dogs.