For the first time in U.S. history, more than 100,000 Americans have died from opioid overdose in a 12-month period from April 2020 to April 2021, according to a report from last November from the Center for Disease Control and Prevention (CDC). Most data from each state show similar patterns as the national trend, from populous states like California to less populated states like Montana and Vermont.
Within states, trends tend to differ among counties. For example, while King County officials in Washington state reported similar trends compared to the national levels, data from Snohomish Overdose Prevention has been seeing a downward trend in opioid-related deaths in the third quarter of 2020. In the bigger picture, however, the rollercoaster trend of such deaths nearly tripled from the first quarter of 2016 to the second quarter of 2020.
In response to the alarming statistics, the CDC proposed new guidelines for pain medication prescriptions. These include allowing physicians to judge when to start and continue opioid treatment for individual patients with chronic pain, establishing realistic treatment goals, and giving patients options for nonopioid treatments, such as exercise, psychological interventions, and physical therapy.
“Anytime we experience a trauma or injury, our nervous system and body will go into protection-mode as part of a built-in survival mechanism,” Dr. Kaeli Gockel said, who is a doctor of physical therapy at Swedish Hospital in Seattle, Wash., a graduate from the University of Washington School of Medicine. “For example, after a car accident, we get neck pain because the muscles experience a tremendous stretch that damages the tissues. The same thing can happen in the pelvis after a trauma, such as infection, childbirth, hysterectomy, endometriosis, things like that.”
Dr. Gockel added that guarding—an automatic tightening of the muscles in response to a certain stimulus—can also compound chronic pain, which can bring the pain in a vicious cycle.
“And so, people have chronic pain every time they go to a gynecologist or every time they have penetration with their partner,” Dr. Gockel said. “Even the thought of that activity, their muscles are starting to guard and protect in anticipation of pain, which makes the pain worse, and which makes the guarding worse.”

I was just drawn to this field. It’s underserved and they’re happy to find a provider who can address their problem.” ~ Dr. Kaeli Gockel, owner of thekegel.com. (Photo courtesy yof Kaeli Gockel, DPT)
With the right therapist, physical therapy can be a launch pad for chronic pain patients to start their recovery. Dr. Elliot Feldman, who is a doctor of physical therapy at the University of Washington Medical Center Northwest Hospital’s outpatient center, said that physical therapists provide education, progressive activity and exercise programs that “gently nudge” patients to more pain tolerance and less pain.
“Research is showing that [physical therapy] provides the essential strategy towards recovery and is more often successful in the long run compared to current standards of care,” Dr. Feldman said. “It isn’t as often utilized in a system that quickly guides individuals in pain towards medication, imaging, injections and surgery, but it is a superior first step when you start to notice pain that is impacting your life.”
Rather than thinking that pain is something to avoid or get rid of, Dr. Feldman said that the goal is to reframe how patients think about their pain, which is something that they can adapt to their lifestyle.
He added that hands-on care is best used during the first few months of an acute injury, but it tends to offer little relief in managing chronic muscle and joint pain. Instead, Dr. Feldman suggests that exercise and education are the cornerstones of a strong physical therapy program.
“Pain is not a pleasant experience and often makes people feel that someone doesn’t understand them or there is no way out,” he said.
With the COVID-19 pandemic still lingering, not everyone feels safe or is able to go see a physical therapist in person: this is where telehealth comes in. Physical therapists are still able to do evaluations, such as range of motion and muscle strength, from a video call.
“Patients really enjoy it because [telehealth] gives them more flexibility in time, especially new moms since childcare has been more difficult during the pandemic,” Dr. Gockel said, who also provides private telehealth for pelvic pain patients. “It allows them to stay home while still being able to get to their PT appointment.”
“The vast majority of my patients with chronic [muscle] pain meet with me via telehealth and rarely come into the clinic,” Dr. Feldman said. “Telehealth has been reimbursed because of an emergency order with the pandemic for physical therapy but hasn’t been permanently established. My hope is that it will be a permanent thing, but I worry that the perception of the physical therapy majority of hands on care will potentially affect the probability.”

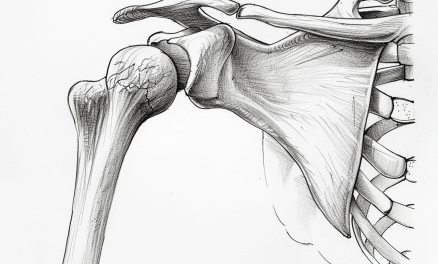
New guidelines from the CDC emphasizes alternative treatments to opioids for chronic pain, such as physical therapy and exercise. Photo by Penny Goldberg, DPT, ReQuest Physical Therapy
With the CDC shifting its guidelines to a more holistic approach, many physical therapists like Dr. Feldman and Dr. Gockel are optimistic about being part of the solution to the opioid crisis.
“What we do has to do with human dignity. It’s a basic human function,” Dr. Gockel said. “Helping patients manage their pain and get back to participating in activities of daily living again is a huge deal and that is why I was just drawn to this field. It’s underserved and patients are happy to find a provider who can address their problem.”
The CDC encourages the public to comment on the opioid guidelines update via the Federal Register docket, which is open until April 11, 2022.
Further reading: [How Massage Therapists Can Work With Pelvic Pain Physical Therapists]
Feature photo: K.C. Alfred/San Diego Union-Tribune/TNS
A native of San Diego for nearly 40 years, Nick Ng is an editor of Massage & Fitness Magazine, an online publication for manual therapists and the public who want to explore the science behind touch, pain, and exercise, and how to apply that in their hands-on practice or daily lives.
An alumni from San Diego State University with a B.A. in Graphic Communications, Nick also completed his massage therapy training at International Professional School of Bodywork in San Diego in 2014.
When he is not writing or reading, you would likely find him weightlifting at the gym, salsa dancing, or exploring new areas to walk and eat around Southern California.