There seems to be a never-ending parade of stories and articles in social and mainstream media about pain caused by some sensory or structural factor. Claims about too much tension in your psoas could pull your pelvis out of alignment, “poor” posture causes back pain, and text neck litter cyberspace and print like confetti throughout Times Square after the New Year’s Eve countdown. Usually, these stories end with a link to the author’s or someone else’s website that provide a “solution” to the “problem.”
Since the 1950s, pain science has evolved quite rapidly and grew more complex, moving away from the Cartesian model of pain that has been the foundation of pain treatment for over 300 years. Current research integrates biology, neuroscience, psychology, genetics, sociology, and other disciplines of science and humanities into understanding pain, which guides clinicians to choose better and efficacious treatments.
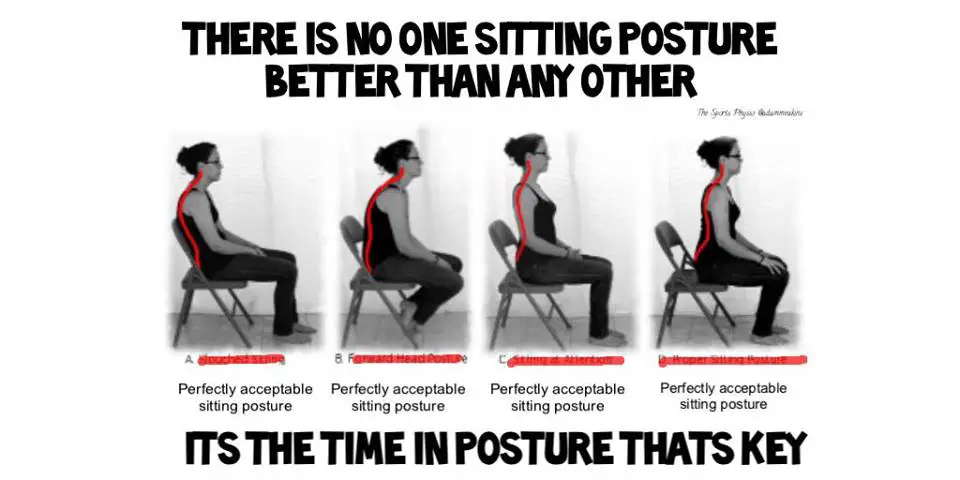
Research has found little or no evidence in a variety of biomechanical factors that are the primary contribution to pain, such as disc hernia in the spine, leg-length discrepancy, anterior pelvic tilt, and spinal curvature. Even one small study found a higher prevalence of back pain among cricket players with higher body symmetry than those with higher body asymmetry.
With a body of scientific knowledge of pain (1) that constantly evolves and changes with newer and evidence, why are so many manual therapists and trainers and most of the public are still entrenched in the “posture = pain” model? The point of this article is not to provide evidence behind the biopsychosocial model of pain or refute the Cartesian model of pain; instead, we examine why such myths still prevail and what we — as professionals — can do to educate the public and our clients and patients about pain.
Let’s Start With Pain Education
Eyal Lederman, who is an osteopath from London, mentioned in a podcast that most manual therapy education is rooted in anatomy and lack an understanding of other aspects of human body, such as motor control and timing.
“How many manual therapy courses, including osteopathy and chiropractic training, do you see people learning about motor control and movement control? Next to nothing. The focus most of the time is on anatomy, and quite often if they are faced with some kind of clinical conundrum, they would go back to their anatomical text books quite often to try to solve it, [which is] why the person is not getting better.”
Therefore, it is easier to reduce the problem down to a single source (e.g. psoas, the “core,” glute medius) rather than understanding the intricate relationship of how the biology, psychology, environment, and social settings affect patients’ pain perception. Therapists and trainers who primarily study the “meaty” parts of the human body would have a “meaty” solution to the problem.
It is also an easier concept to sell and market a service or product. There are courses that teach you how to “release fascia” with your bare hands or design exercise programs to strengthen or lengthen muscles to “correct” posture or “imbalance.” There are products like colorful sticky tapes or bracelets that take the back or knee pain away.
“It’s a little bit like you break up things so you can sell them off individually. That’s how it works. It works in fads, a lot of this stuff,” said Lederman. “It used to be that the abdominus. Now it’s the foot, core muscles, it was then the latissimus, and then there’s a whole system develops around that. There is a commercial element in it.”
Words and Listening Matter For Someone in Pain
Posture and other biomechanical factors aren’t the only things affecting pain. Emotions can affect how patients and clients perceive and understand their pain and how satisfied they are with the treatment and findings, which may increase the likelihood that their pain could be reduced. A 2013 study that was published in Clinical Orthopaedics and Related Research found that 70 percent of the sample population (n=100) prefer clinical reports that were easier to read and simpler than reports with more technical terms. (2)
“Subjects felt more pleasant, calm, and in control on average after reading MRI reports reworded for readability and optimism. They also rated the reworded reports as more satisfying, useful, and understandable on average. Most patients preferred the reworded report over the original report,” the researchers wrote. However, the remaining 30 percent of sample stated that the simpler version was “too simple” and prefer to decipher the report on their own with the internet or with their physician.
Another Swedish study with 28 nurses with low back pain published in the European Journal of Pain found that those who were validated had “significantly decreased their sadness, anger, frustration and pain after they had been interviewed” while those who weren’t validated had higher levels of frustration after the interview. (3)
“The present study showed that people who experience back pain and are interviewed and treated with validation, tend to lower their levels of negative affect and pain. In addition, they are more satisfied than people with pain that are met with invalidation. The clinical implication is that patients with back pain would benefit from physicians using more validating communication styles,” the researchers concluded.
These are just two out of many studies and reviews that examine the psychosocial factors that often gets ignored in manual therapy and fitness education when it comes to dealing with pain.
“There is great data on this: Stress, distress, and less effective coping strategies explain more of the variation in symptom intensity and magnitude of limitations than any type of pathology or impairment,” explained Dr. David Ring, Professor of Orthopedic Surgery at Harvard Medical School, in an email correspondence with Massage & Fitness Magazine. He is also one of the researchers in the MRI study.
“People seek coaching for diet; coaching for fitness; coaching for sports. Coaching for mindset is the great untapped resource for health because good health isn’t having a certain type of body. Good health is being able to depend on the body that you have.
“The real problem is that in my clinic I get patients that come in with back pain, that have been to therapists other than me, and the condition has been pathologized to a new degree. They are now told that they’ve got flat feet, and that’s why they’ve back pain, their pelvis is rotated, their core muscles are not working anymore.
“They are weak, and unless they do something about all this, they’ll never get better. That’s the real problem, so what we are doing is what we blame sometime the medical profession in doing is that we pathologize it even further, simple things.”
“You can imagine a patient comes to us. They’ve only got a back pain. They’re worried about a back pain, and now they’ve got to worry about their posture, they’ve got to worry about their pelvis, and they’ve got to worry about their core muscles not working very well.” ~ Eyal Lederman, DO
If more therapists and trainers recognize the basics of current pain science, then we would likely see a reduction of quick fixes and myths permeating in the media and better client or patient outcomes when it comes to pain. We would understand that emotions, experience, and other psychosocial factors contribute to pain, not just the biological parts. There is no need to put clients and patients in a merry-go-round of seeking and getting ineffective treatments or heavily relying on the therapist or trainer.
But it won’t be easy to change someone’s mind about what they believe and experienced in the gym or clinic. Part Two will go over the communication issues.
References
1. Melzack R, Katz J. Pain. WIREs Cogn Sci. 2013 Oct; 1–15. doi: 10.1002/wcs.1201.
2. Bossen JK. Does rewording MRI reports improve patient understanding and emotional response to a clinical report? Clinical Orthopaedics and Related Research. 2013 Nov;471(11):3637-44. doi: 10.1007/s11999-013-3100-x. Epub 2013 Jun 13.
3. Vangronsveld KL, Linton SJ. The effect of validating and invalidating communication on satisfaction, pain and affect in nurses suffering from low back pain during a semi-structured interview. European Journal of Pain. 2012 Feb;16(2):239-46. doi: 10.1016/j.ejpain.2011.07.009.
A native of San Diego for nearly 40 years, Nick Ng is an editor of Massage & Fitness Magazine, an online publication for manual therapists and the public who want to explore the science behind touch, pain, and exercise, and how to apply that in their hands-on practice or daily lives.
An alumni from San Diego State University with a B.A. in Graphic Communications, Nick also completed his massage therapy training at International Professional School of Bodywork in San Diego in 2014.
When he is not writing or reading, you would likely find him weightlifting at the gym, salsa dancing, or exploring new areas to walk and eat around Southern California.