Pudendal neuralgia is the irritation, entrapment, or compression of the pudendal nerve, which can cause a sharp pain along the path of the nerve. It starts from a bundle of nerves from the sacrum, curving around the sciatic foramen of the pelvis and toward the genitals and rectum. There, the nerve branches out to three areas:
- dorsal nerve: innervates the genitals
- rectal nerve: innervates the external anal sphincter
- perineal nerve: innervates the perineum, scrotum, labia major
Also, the pudendal nerve is a bundle of sensory, motor, and autonomic nerve fibers, kind of like a coax cable with different kinds of wires inside. Given its anatomy, it’s no surprise that pain coming from the pudendal nerve could be a cause of pelvic pain. However, it is quite rare—about 1 out of 100,000 people gets it where 2 out 3 of three cases are women.
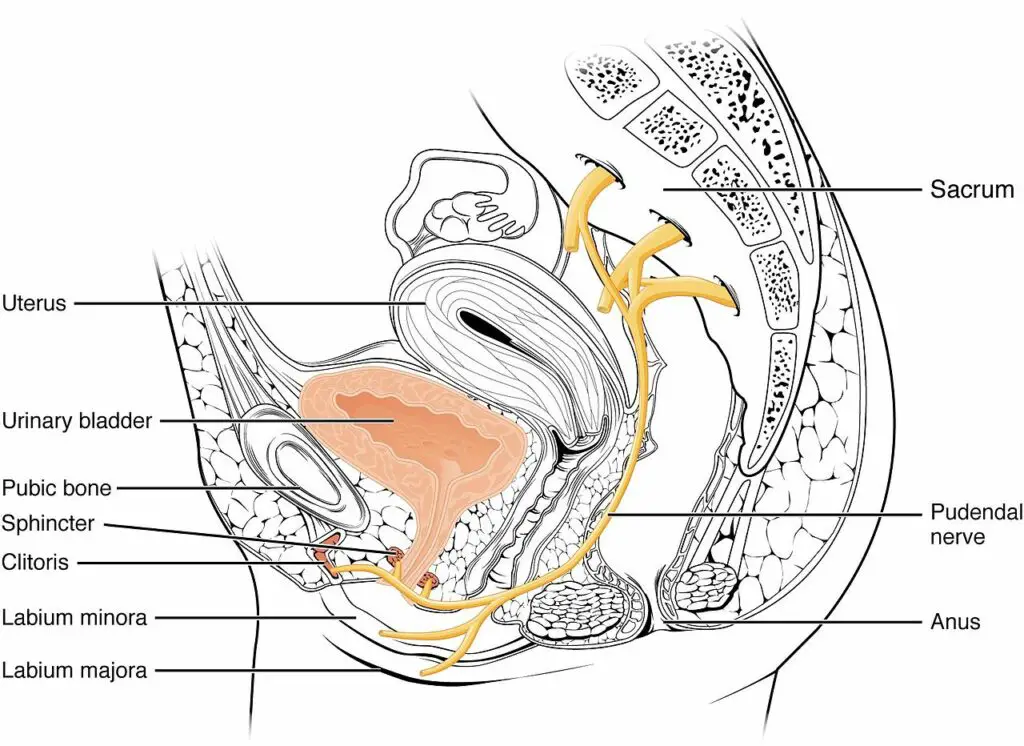
The pudendal nerve innervates organs and other tissues in the lower pelvic region, including the: lower buttocks. area between the buttocks and genitals (perineum) rectum, and anus. (Illustration by OpenStax College, distributed under Creative Commons Attribution 3.0 Unported license.)
The word “pudendal” mean “to be ashamed” in Latin, which is also an archaic term that refers to anatomy near the genitalia, like the pudendal artery. Oftentimes, this type of nerve pain caused by sitting or cycling for too long, childbirth, or pelvic surgery, which can cause pain during urination, defecation, and sexual intercourse. But with the right medical care, pudendal neuralgia exercise may help alleviate pain and improve pelvic function.
Does exercise work for pudendal neuralgia?
Because pudendal neuralgia is often caused by nerve entrapment or compression at the pelvic floor, exercise can increase muscle and nearby connective tissue extensibility, which may loosen up the nerve’s area.
Some research shows that stretching, aerobics, and strength training can reduce pelvic pain for pudendal neuralgia and other types of nerve entrapments. However, some of the evidence is based on six cases, which may not apply for the general population.
Also, just working out has been shown to reduce general pain due to exercise anesthesia where your brain generates more natural painkillers like endorphins. While not everyone can enjoy or perform the same exercises, you should find the ones that you can do with little or no pain.
Pelvic floor relaxation exercises
These exercises target your hip area to help decompress the nerve and strengthen the pelvic floor. They are based on what some researchers have found to be effective for a small population of people. Check with your physical therapist or healthcare provider for a more specific exercise program. These should be done twice a day—morning and night.
Supine hip rolls
- Lie on your back with your feet on the floor about hip-width apart.
- Exhale as you lift your buttocks off the floor.
- Gently roll your hips side to side once, return to the center, and lower your buttocks to the floor. Do 8 to 10 reps.
Low back stretch
- Lie on your back with your feet together.
- Raise one knee toward your stomach and grab your knee with both hands.
- Exhale as you lift your head and shoulders off the floor as you gently pull your knee to maintain the position.
- Hold this position for about 4 to 5 seconds, and return to the starting position.
- Repeat the exercise on the leg, and alternate between leg for about 5 to 6 reps.
Quadruped spine flexion and extension
- Go on all fours with your hands and knees on the floor. Your hands should be below your shoulder joints, and your knees should be below your hip joints.
- Exhale as you bring your right knee toward your chest. Flex your neck as you do so.
- Exhale as you extend your right leg behind you as you raise your head up.
- Perform 8 to 10 times per leg.
Sit-ups
- Lie on your back with your feet flat on the floor about hip-width apart.
- Lace your fingers behind your head, and exhale as you lift your shoulders and upper back off the floor as much as you can.
- Lower your body back to the starting position, and perform 10 to 12 reps.
Full-body strength exercises
These typical gym exercises not only strengthen your hips and lower body but also likely induce exercise analgesia—moreso than the relaxation exercises.
Barbell Squats
Whether you’re using a barbell, dumbbells, or even a sandbag, all squats improve strength and stability in your hips, abdominals, and legs.
For front squats with a barbell, you may need to reduce your weight by at least half.
Deadlifts
Deadlifts primarily work on your buttocks, hamstrings, and abdominals. You can do this in a variety of ways, including:
- standard deadlift
- sumo
- single leg
Depending on the type of deadlift, you can do these with a barbell, kettlebell, or a dumbbell.
Lunges
Lunges can be done in various planes of motion: to the front, to side, and with a turn or rotation. You can do these with weights in your hands or no weights.
Leg press
Like the squat, the leg press strengthens your lower body. The benefit is that there’s less concern about maintaining your balance, and it’s easier to change the weight than with a barbell.
Pudendal neuralgia symptoms
If you have pudendal neuralgia, you may feel a sharp pain at or near your genitals when you sit, especially if you sit for a long time. It can also be general pain in your pelvis on one or both sides of your body. The pain can be described as stabbing, burning, achy, pinching, or numbing.
Because pudendal neuralgia is relatively rare and has overlapping symptoms with other types of nerve entrapment, it can be mistaken for urinary problems in men and gynecological problems in women.
“The pudendal nerve is the main sensory nerve to the bottom of the pelvis. It is responsible for sensation around the anus and external genitalia,” said Dr. Ken McGee, who is a physical therapist practicing in Mill Creek, Wash. “When this nerve has been injured, sensation can be disrupted throughout the pelvis. For some, this disrupted sensation results in numbness at the bottom of the pelvis, but for many other people it presents as crushing pain. Clients may describe the feeling that a bowling ball is coming out of the pelvis.”
McGee also pointed out that many people with pudendal neuralgia develop depression and anxiety, and depression has been shown to be a predictive factor for those who do not respond to nerve blocks.
For physicians, the best guidelines to date is the Nantes Criteria, which was developed in 2006 by a group of physicians in France. The criteria for diagnosing pudendal neuralgia are:
- Pain from the anus to the clitoris or penis
- Pain from sitting (even if it’s just sitting on the toilet long enough to take care of business)
- Pain doesn’t wake you up at night
- Pain is taken away by a nerve block
- Pain doesn’t affect sensory function, such as the sphincter.
Other treatments for pudendal neuralgia
If exercise doesn’t work for you, there are other options to treat pudendal neuralgia.
Physical therapy
Physical therapy for pelvic pain involves a combination of soft-tissue manipulation, joint mobilization, exercise, taping, electrical stimulation, and/or other types of non-invasive treatments.
When you go see a pelvic pain physical therapist, you can expect them to:
- review your health and lifestyle history thoroughly
- evaluate your symptoms and areas that you feel pain
- conduct a movement assessment of your hips and other body parts
- provide a customized treatment plan that may take six to 12 weeks
Despite the recommended exercises that were mentioned earlier, there’s no strong evidence that shows they are strongly effective in reducing pain from pudendal neuralgia on a population basis. The most recent review stated that “there is too much variability” in the evaluation and techniques to come up with a conclusion.
Aside from exercises and various passive treatments, McGee recommended that manual therapists start with educating their patients or clients about their condition.
“My experience with treating pudendal neuralgia is that is requires a team approach. The ideal team may include a mental health therapist, possibly a psychiatrist too, as well a physiatrist for injections,” McGee said. “If a client is interested in pudendal nerve decompression, then a surgeon is also part of the team. The manual therapist has a large roll to play in addressing discomfort in soft tissues either directly impacted by disrupted nerve function, or in surrounding muscles that compensation for movement and activity changes. Depending on scope, a manual therapist may also provide guidance on movement and body mechanics.
“There is limited evidence on specific manual therapy interventions for pudendal neuralgia. Accordingly, manual therapists must listen to a client’s story and goals to develop a plan for reducing soft tissue pain.”
Cushions

Photo courtesy of Dr. Ken McGee.
Some types of cushions can help make sitting more tolerable, said McGee, such as coccyx cushions. These have a cut out to take pressure off the pudendal nerve. “Many people are also able to make do with two pillows with a gap in between or two folded up towels with a gap,” they said.
Electrical stimulation
Transcutaneous electrical nerve stimulation (TENS) provides mild electrical currents to alleviate pain. Based on the gate control theory of pain, the electrical stimuli from TENS activate certain sensory organs in the spinal column that block electrical signals that increase pain sensitivity.
While the scientific evidence behind its efficacy is so-so, TENS and similar electrical treatments may help certain individuals for temporary pain relief without relying on medications and frequent visits to their therapist.
Medication
There is no known medication that is specifically for pudendal neuralgia. But for general neuropathic pain, a 2020 systematic review suggested three types of medications:
- duloxetine and venlafaxine: both antidepressants have been shown to be highly effective compared to a placebo. Commonly reported side-effects include nausea, loss of appetite, somnolence, asthenia and dry mouth. Caveat: people with multiple sclerosis have high dropout rates from duloxetine studies compared to those who get a placebo.
- gabapentin: an antiepileptic drug that has been shown to be more effective than a placebo, but it may not work in an emergency room situation.
Other medications, such as pregabalin and clonazepam are “inconclusive,” while opioids should be avoided because of their highly addictive nature.
Please check with your doctor for your specific medication. Do not self-medicate.
Psychotherapy
Oftentimes, chronic stress, depression, anxiety, and trauma can be major factors that influence the degree of pain. One common type of psychological treatment is cognitive behavioral therapy (CBT), a form of “talk therapy” that helps you sort the way you think about your problems with the help of a mental health therapist.
While there’s no known research that specifically targets pelvic pain, the current consensus suggests that CBT can be part of the total treatment for pudendal nerve pain if you have at least one mental health problem diagnosed.
Surgery
Surgery is often used as a last resort if all non-invasive procedures fail, and only if you have pudendal neuralgia for at least one year. This would involve making more space for the pudendal nerve to move while maintaining its stability.
The surgery may be done if one of four ways, depending on where the symptom(s) come from:
- transperineal: procedure is done via the perineal muscle
- transgluteal: procedure is done via the gluteal muscles
- transischiorectal: procedure is done near the rectum and/or the ischium
- laparoscopic: procedure is done via the abdomen
Current evidence shows that most surgeries have a 60% to 80% success rate. Also, all five factors based on the Nantes Criteria must be present before a surgeon can consider you for surgery.
“Just remember that each and every case is so different and the assessment and plan must be individualized. I find that so often people go online and see similar symptoms and run out and have unnecessary procedures. Find someone who understands this.” ~ Dr. Tracy Sher
Does massage work for pudendal neuralgia?
Massage therapy might alleviate the symptoms of pudendal neuralgia, but most practices prohibit the treatment near or at the genitalia. But standard massage therapy on the lower back, glutes, and legs—including sports massage—can alleviate pain temporarily. The relaxation effect that it provides can decrease stress and “calms” the nervous system, which decreases pain sensitivity. This may help you sleep better and as part of stress management.
If you choose massage therapy as a part of your treatment, make sure it doesn’t provoke further pain and your therapist should understand your situation before treatment.
“Any client that has pudendal neuralgia should be referred to a mental health provider if they are not already seeing one. Manual therapists can use tools such as Psychology Today’s Therapist Finder Tool or Open Counseling,” McGee suggested.
Resources
A native of San Diego for nearly 40 years, Nick Ng is an editor of Massage & Fitness Magazine, an online publication for manual therapists and the public who want to explore the science behind touch, pain, and exercise, and how to apply that in their hands-on practice or daily lives.
An alumni from San Diego State University with a B.A. in Graphic Communications, Nick also completed his massage therapy training at International Professional School of Bodywork in San Diego in 2014.
When he is not writing or reading, you would likely find him weightlifting at the gym, salsa dancing, or exploring new areas to walk and eat around Southern California.