Ehlers-Danlos syndromes (EDS) describe a group of connective tissue diseases or disorders that affect the body in many ways. It’s often associated with joints that move beyond normal range of motion to the point of potential subluxation or dislocation.
EDS has a genetic component (passed from parent to child) that changes the structure and function of collagen and some connective tissue proteins.
Scoliosis, joint deformities, skin hyperflexibility, hernias, and other structural weaknesses can be associated with EDS. The rarer types of EDS may also come with weakness in specific tissues that can lead to disease of the gums or eyes, cardiac disorders, and ruptures of the abdominal organs, uterus, or blood vessels.
Most connective tissue disease diagnoses are not easily made. Mixed connective tissue disease (MCTD) is one of many autoimmune diseases, such as scleroderm and rheumatoid arthritis, where the body attacks its own healthy cells.
Patients with MCTD have features of more than one autoimmune disease and test positive for the anti-RNP antibody. Those with features of multiple autoimmune diseases that don’t have the antibody are classified as having “overlap syndrome,” which is having two or more recognized autoimmune diseases.
At times, patients can have symptoms and lab test results suggestive of connective tissue disease without enough characteristics to be grouped into one of the well-defined diseases, such as rheumatoid arthritis, lupus, or scleroderma. These patients are diagnosed with “undifferentiated connective tissue disease.”
Living and working with EDS can be challenging. Even the simplest, most mundane tasks can be difficult and harrowing. Rob Haddow, the owner of Rob Haddow Massage Therapy, is a registered massage therapist in OakVille, Ontario, who is navigating EDS one day at a time.

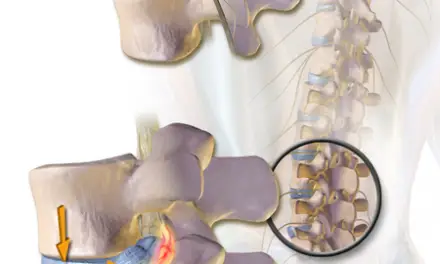
Rob Haddow demonstrates how nerves affect movement of the ankle joint and how pain affects those with Ehlers-Danlos syndrome. Photo courtesy of Rob Haddow.
For him, managing EDS varies from day to day. He starts his day by checking his joints for dislocations. Once he has ensured everything is in place, he spends a few minutes assessing his tolerance (or intolerance) to movement.
“I’ll check for spasms on lumbar extension or see how much dorsiflexion my left ankle has available,” Haddow said. “Recently, my right shoulder has been the most problematic with regular dislocations during the night, so I wake up and check on that.”
After checking in with his body, he can either start his day or spend some time working on rehabilitation-based movement and exercise.
Erica DeNeve, a registered massage therapist at Whyte Avenue Chiropractic and Wellness, in Edmonton, Alberta, also lives with EDS. She spends her mornings working up the energy to shower, dress, eat, and walk her dog.
“I have chronic migraines, insomnia, and mild dysautonomia,” DeNeve said. “I average four hours of sleep a night and my pain is usually a 4 on a standard pain scale. When I get a migraine, it can increase to 7 or 8, but they only last a few hours.”
She has been working five, four-hour days as a massage therapist for more than 20 years and has become accustomed to the pace. DeNeve, along with most people with EDS, has a host of co-morbidities along with pain.
What are the different types of EDS?
There are three common types of EDS: classical, hypermobile, vascular.
Classical EDS
Classical EDS is well-known for skin hyperextensibility and joint hypermobility. Lesser-known symptoms include smooth skin that easily bruises, fragile tissues, and family history.
Patients may also have molluscoid pseudotumors that tend to form over pressure points such as the elbows and knees or subcutaneous spheroids (small calcified nodules) may form under the skin.
Hypermobile EDS
Joint hypermobility and loose, stretchy, velvety skin is also associated with hypermobile EDS although to a lesser extent than in the classical presentation. This presentation is the most debilitating in terms of musculoskeletal symptoms with 100% of patients reporting joint pain.
Those with hypermobile EDS have lax ligaments that start very early in development but don’t see an onset of pain until they’re in their 20s. This chronic pain and instability limit daily activities, and it eventually gives way to a stiffness phase that limits motion in the peripheral joints and spine.
Vascular EDS
This is the most serious type of EDS. Vascular EDS is marked by the fragility of the organs and can have significant consequences, including rupture of the arteries, intestines, or uterus.
Other signs of vascular EDS may include thin, translucent skin where the underlying vessels are visible. Wrinkling of the handles and feet is common due to the loss of subcutaneous fat in these patients.
Patients with vascular EDS typically have a slender face and lobeless ears. They may have small joint hypermobility but are less likely to have such hypermobility in larger joints and skin extensibility.
Other Types of EDS
- Classical-like: similar to classical EDS in presentation but patient meets additional major criteria of having skin that bruises easily
- Cardiac-valvular: problems with heart valves (aortic, mitral), hyperextensible skin, atrophic scarring, thin skin that bruises easily, and joint hypermobility
- Arthrochalasia: congenital bilateral hip dislocation, severe joint hypermobility, and skin hyperextensibility
- Dermatosparaxis: very rare (15 cases as of 2017), patients have very loose, fragile skin that is easily bruised. Most with the condition have distinct facial features (prominent, protuberant eyes, excessive skin around the eyes, undersized jaw)
- Kyphoscoliotic: congenital decrease in muscle tone, congenital scoliosis, and joint hypermobility particularly in the shoulders, hips, and knees
- Brittle cornea syndrome: Major criteria are thin cornea, keratoconus, keratoglobus, and blue sclera (the part of your eye that is normally white)
- Spondylodysplastic: characterized by short stature, decreased muscle tone, and bowing of limbs
- Musculocontractural: diagnostic criteria include congenital contractures (typically adducted thumbs, clenched fists, and/or clubfoot), craniofacial features (flat skull, wide-set eyes, strabismus, prominent nose, thin upper lip and small mouth, etc.), and skin hyperextensibility as seen in other types of EDS
- Myopathic: congenital muscle atrophy and hypotonia that improves with age, joint contractures (hip, knee, and elbow), and hypermobility of distal joints (wrists, ankles)
- Periodontal: major criteria are severe periodontitis from an early age, unattached gingiva, pretibial plaques, and family history of a first-degree relative
What causes Ehler-Danlos syndrome?
Most forms of EDS are caused by genetic mutations that change the body’s collagen production. While the affected genes have been identified in the classical (COL5A1, COL5A2, or COL1A1) and vascular (COL3A1) forms, scientists have yet to find the origin of the other forms.
These conditions are often inherited through autosomal dominance (passed from parent to child). Collagen gives our body structure and is a basic component of muscles, tendons, bones, vessels, and skin.
In most people, collagen is abundant in these tissues, but in people with EDS, there may be less collagen or the collagen they do have may be weak.
What does EDS pain feel like?
The pain experienced by those living with EDS can be as variable as the presentation of the disease itself.
DeNeve describes her pain as diffuse and constant. Her daily pain is rarely specific to a muscle or joint the way we might expect with a musculoskeletal injury (i.e. posterior leg pain with a hamstring strain) but following a joint dislocation or subluxation, the pain may follow more typical symptoms.
For Haddow, pain is difficult to describe despite being an everyday part of his life. He has had pain for as long as he can remember. Haddow has had a host of injuries associated with his EDS and finds the muscle spasms to be worse than most orthopedic injuries.
“I experienced a compound fracture of my shin, reduced it, and found that it was less physically uncomfortable than my back spasm that morning,” he recalled.
He acknowledged that his scale is skewed without knowing why.
“Some physically traumatic experiences I have had were relatively innocuous to me, while some others have been significantly more impactful,” he said.
What is the life expectancy of someone with Ehlers-Danlos syndrome?
In those with classical and hypermobility forms of EDS, a normal lifespan can be expected.
Vascular EDS, the most severe form, has a life expectancy of 48 years with most having a major event by 40. Similarly, those with kyphoscoliosis may have vascular involvement and restrictive lung disease which alters lifespan.
A Danish study of more than 1,400 patients over 12 years, with all types of EDS, found the average age at death was 53.6 years.
How is EDS diagnosed? And what is the Beighton score?
Ehlers-Danlos syndrome is diagnosed using a combination of patient history, signs and symptoms, and physical and diagnostic testing. Most physicians should be able to diagnose this condition.
After taking a thorough medical history, the physician will likely assess joint mobility using the Beighton Score (sometimes called the Beighton scale).
The Beighton Score
The Beighton score is a 9-point scale used to measure joint hypermobility. Patients are given 1-point for each maneuver they can do (1-point per side for things done on the right and left).
The maneuvers are: forward bending to touch the toes, hyperextension of the 5th fingers (pinky), touching the thumb to the forearm, knee hyperextension, and elbow hyperextension.
But recent research have questioned the validity of the Beighton score system. A 2021 review by Malek et al. found that many patients with general joint hypermobility may be underdiagnosed for EDS. The scoring system is heavily biased in the upper limbs and has an arbitrary cut-off point that determines if you have EDS or a similar type of disorder or not.
More rare presentations of EDS may be diagnosed using skin biopsy, electron microscopy, urinalysis, and genetic marker testing.
Other physical tests, such as assessing skin mobility and observing for abnormal scarring, can also be helpful. The Ehlers-Danlos Society developed a comprehensive diagnostic screening tool that physicians across all disciplines can use.
Dr. Mike Makher, a physical therapist who specializes in EDS at Good Health Physical Therapy and Wellness in Portland, Oregon, noted that diagnosing EDS can sometimes hand patients more than they bargained for.
He recalled patients being referred to him with a diagnosis of “hypermobility” and realized that it falls on him to educate these patients that their hypermobility is part of a larger clinical picture where the signs and symptoms are likely to change over time (i.e. patients with EDS often get stiffer in their 40s).
Although the screening tool is helpful, he cautions that it’s far from perfect.

“Look for clinicians who are going to partner with you in this journey of figuring out how to address your health concerns.” ~ Mike Mahker, DPT; photo: Mike Mahker
Makher didn’t seek out patients with EDS but has grown into his patient population. While he knew he wanted to work with patients in persistent pain, he wasn’t prepared for most of his caseload to have some form of EDS or joint hypermobility.
He’s interested in this population because they “clearly contradict a number of presumptions that are commonly made about patients.”
“My patients have a genuine pathological concern, however, in addition to the pathoanatomical concerns and co-morbidities (POTS, MCAS, fibromyalgia), they have a number of neurological and psychosocial concerns,” Mahker said.
He recalls the biopsychosocial model of clinical care and states that his patients are a “fantastic example of explicit biological, social, and psychological factors” all presenting in the same condition.
“The cases involving these patients are not super straightforward as they often are coming in after having been traumatized by numerous clinicians,” Makher said. “They’re often called hysterical women, making things up, drug-seeking…the list goes on and on.”
Is massage good for EDS?

Massage therapy can help manage EDS symptoms and provide a more positive well-being for the patient. The type of massage you do depends on the patients’ preferences and condition. Photo: Marie Zahn
Massage therapy can be helpful in managing the symptoms of EDS. That said, patients with vascular EDS may need to skip massage because of the potential complications associated with blood clots.
In classical EDS, massage therapists should be extra cautious with the patient’s fragile skin.
There are some general guidelines for working on patients with EDS. One comprehensive approach to physical and manual therapy is the Muldowney Protocol.
The Muldowney Protocol was presented at the 2019 EDS Global Learning Conference. Developed by Kevin Muldowney, a physiotherapist with more than 10 years of experience treating patients with EDS, the protocol is geared toward assisting therapists in finding their place with these patients.
Muldowney’s treatment philosophy emphasizes that exercise is the only treatment that provides lasting results. Manual therapy, including massage therapy, can be used to decrease muscle spasms, inflammation, and pain.
He includes the caveat that manual therapy should not be performed on a joint that is not also being strengthened because of the potential for stability issues.
DeNeve echoes those sentiments when it comes to her own management.
“Because our joints are so loose, our muscles are much tighter than the average person’s,” she said. “Tension is released too much, we become unstable.”
She cautioned that massage therapists and physical therapists should be careful not to take joints to their end range where subluxation or dislocation is possible. High pain levels and over-excited nervous systems are hallmarks of all subtypes of EDS.
DeNeve said that these patients tend to suffer from high levels of depression and anxiety.
“Gentle, compassionate touch can help alleviate symptoms of all of those problems,” she said.
Are there massage techniques used for EDS patients?
DeNeve recommends dermoneuromodulation for her patients. As the name suggests, “dermoneuromodulation” means using the skin and nerves to create change.
This approach is non-painful as it uses light to moderate pressure over the targeted area for several minutes. It’s believed that the same nerve that innervates the joint and muscles, also provides input to and from the skin.
As such, the movement of the skin that stretches the nerve can affect all aspects of the musculoskeletal system.
Once a tender area has been located, the therapist applies a light stretch to the skin to provide relief.
Haddow also uses a lighter touch with his patients. His reasons for this are three-fold: his patients prefer it, it allows him to preserve his own body while working, and it helps!
Manual therapy can be used to calm the nervous system as well as manage pain. Depending on a patient’s unique response, he may be completely hands-on or use mixed modalities to treat his patients.
“Some of my treatment sessions may be minimally or majorly hands-on depending on pain at that time and whether that individual’s pain responds to manual work,” he said.
Haddow sums up his approach to treatment quite simply. “Generally, I’ve found a mix of remedial exercises to be helpful on days of high tolerance while manual work seems to be helpful to gradually challenge and down-regulate sensitivity on days of low tolerance.”
Are there contraindications of massage for EDS?
As mentioned earlier, techniques that take a joint to end-range are contraindicated in most everyone with EDS. Relative contraindications vary widely from patient to patient and one type of EDS to another.
Manual therapy and massage are mostly safe for patients with EDS. However, there’s no one-size-fits-all approach.
“Just because a patient has EDS doesn’t mean they are globally hypermobile,” Haddow said. “It is prudent that all therapists obtain a thorough health history including the global presentation and the day-to-day signs and symptoms of EDS.”
Makher emphasized the need for patient education through careful word and intervention choices. He worries that creating patient dependence on massage or manual therapy can have detrimental long-term effects.
“Manual therapies can be useful for temporary pain relief and to help relax muscles for short-term periods,” Makher said. “Nothing wrong with getting a massage if you like it. The narrative needs to be clear that it’s not a fix and one shouldn’t become dependent.
“I’ve seen patients get so dependent that they’re seeing the same PT, chiropractors, and massage therapists for almost nothing but manual for 2, 4, 5, even 8 years.”
Haddow and DeNeve suggested that you should avoid seeing therapists who see themselves in a healer/guru role rather than a member of a multidisciplinary treatment team.
Haddow relayed a story of his own massage experience with a therapist who wasn’t willing to listen to him.
“I had a [massage therapist] who would insist that I needed techniques that I abhor because they would help with ‘alignment’ or ‘scar tissue and adhesions,’” he said. “It made for some of the most unpleasant massage treatments I have ever experienced.”
Patients should view working with therapists who are misinformed, unwilling to accept new information, or judgemental as contraindicated in their treatment.
“It’s both frustrating and potentially dangerous to work with a practitioner like that,” Haddow said.
Finding a massage therapist for Ehlers-Danlos syndrome
The million-dollar question. Finding a practitioner who is willing to embrace “flexibility in their dogma” is key, according to Haddow. He said that much of what is taught about EDS is based on information that is evolving, so the therapist has to be open to accepting new ideas in the field. A willingness to learn is paramount.
A massage therapist who listens to the patient is also key. The presentation of EDS is different from patient to patient and day to day, so what was appropriate and effective last time, may not be the best approach this time.
Insisting that a particular treatment approach is the only way to treat EDS often leaves the patient frustrated, unheard, and still in pain.
In DeNeve’s best-case scenario, the massage therapist has not only heard of EDS but has experience treating it. If that’s not possible, a therapist who is willing to research the condition will suffice.
She also emphasizes that the therapist must be willing to listen to the patient.
“Most ‘zebras’ — the name patients with EDS use for themselves — know exactly what their bodies are capable of and need,” DeNeve said.
Does physical therapy help with EDS?

Some patients Ehlers-Danlos syndrome have trouble maintaining balance. Some exercises can help improve their body awareness. Photo: Penny Goldberg.
Although the current evidence base for physical therapy in patients with Ehlers-Danlos syndrome is scant, there are plenty of anecdotal reports of patients who have decreased pain and improved function following an episode of physical therapy care.
Physical therapy can help patients with EDS in several ways. The therapist can focus on improving patients’ joint pain secondary to hypermobility, poor posture, gait deviations, strength and endurance, balance, and learning activity and home modifications to ease the potential burdens of living with EDS.
Physical therapists are movement specialists and can assist patients with EDS in improving how they do activities of daily living. Physical therapy should focus on gentle stretching, along with exercises that promote general strengthening and proprioception.
Makher emphasizes a “test-retest” approach with his patients where every activity is assessed for comfort.
When POTS is present along with EDS, he suggested cardiovascular training as part of exercise. Patients with POTS can start with swimming, rowing, or biking and work their way up to exercising on an elliptical trainer, treadmill, or stair stepper.
Also, many physical therapists specialize in treating chronic pain, which is also prevalent in those with EDS.

Strength training can not only help EDS patients get stronger and more resilient against their symptoms, it can help them feel more empowered and have more agency. Photo: Mike Mahker.
Makher found that a varied approach works best for his patients. He included elements of neuromuscular re-education and strength training to cue the parasympathetic nervous system (read: more rest and digest, less fight or flight) while also maintaining function.
Most physical therapists can treat almost anyone that walks through their door, but it may be beneficial for patients to research providers in their area to see if there are local therapists who specialize in EDS.
“[Search] for clinicians who are going to partner with you in this journey of figuring out how to address your health concerns,” he recommended.
How can you find the best doctors for Ehlers-Danlos syndrome?
Most physicians should be able to make the diagnosis of EDS but this does not mean they are the best for managing the long-term care plan. Once diagnosed, Makher urges patients to steer clear of practitioners who use a “hyper-specific” approach.
A clinician who partners with the patient in the quest to address their health concerns can go a long way. He iterates, “they don’t need to know everything about EDS but they need to be open-minded, collaborative, and respectful of you.”
The EDS society maintains a list of healthcare professionals across all disciplines that is available to patients that can be used as a starting point.
It’s worthwhile to look for state-based or your local EDS support groups where opportunities to learn about clinicians from other patients may be available.
Lastly, he implores patients with EDS to avoid clinicians with a less-than-stellar bedside manner.
“Please don’t accept someone’s advice if all they say to you is, ‘You just need to exercise,” Makher said.
[More about narrative medicine in massage therapy and how that can help you find the right caregiver.]
Living with Ehlers-Danlos syndrome
Learning to live with EDS is a difficult process that can take several years of refinement.
DeNeve has maintained her schedule for more than 20 years thanks to pacing, supplements, and bracing. Magnesium and water with electrolytes help keep her energy up and her body moving.
She suggested investing in (and using!) good braces so that when something is sore or subluxated/dislocated, you are ready to protect yourself from more damage and manage your pain.
Along with Makher, she also suggests finding an EDS support group, such as the one on the Ehlers-Danlos website.
“There are groups that have sprung up all over the globe, and we share information and support and understanding,” DeNeve said.
The American Journal of Medical Genetics makes recommendations for the management of the vascular and hypermobility types of EDS should include:
- minimizing risk of injury to organs/vessels
- creating a care team
- planning for emergency care especially when traveling
- maintaining normal-range blood pressure.
Haddow and DeNeve have decades of combined experience in the management of EDS. They may have the same diagnosis, but their daily management is very individualized.
If nothing else, the take-home message should be that EDS is not a one-size-fits-all diagnosis and you won’t be best-served by a cookie-cutter approach.
Building a team inclusive of physicians, massage therapists, and physical therapists who understand EDS will make navigating this life-long condition a little less treacherous.
Also, the mental challenges that come along with realizing you can’t fulfill the plans you had for the day can be overwhelming at times.
Haddow recommends that you should set yourself up for success by having an alternative plan for the day.
“If I can’t walk very well I have tricks to help with that, and often they help a lot, but I still may not be up to going for a two-hour hike,” he said. “Maybe I’ll go indoor climbing instead and make use of other avenues of movement exploration.”
Haddow also advised that you shouldn’t try to do everything yourself.
“It’s hard as hell to find the right people for your circle of care…even though it can be tiring to keep going, you need to reach out to other Zebras and build those resources,” he said.
“This is not the death sentence it might look like, but it will be hard and take some getting used to,” DeNeve said. “You will be your best advocate. You are not as alone as you think. You can do this.”

Penny Goldberg, DPT, ATC
Penny Goldberg, DPT, ATC earned her doctorate in Physical Therapy from the University of Saint Augustine and completed a credentialed sports residency at the University of Florida. She is a Board Certified Clinical Specialist in Sports Physical Therapy.
Penny holds a B.S. in Kinesiology and a M.A. in Physical Education from San Diego State University. She has served as an Athletic Trainer at USD, CSUN, and Butler University.
She has presented on Kinesiophobia and differential diagnosis in complicated cases. Penny has published on returning to sports after ACL reconstruction and fear of movement and re-injury.
Outside of the clinic, Penny enjoys traveling, good cooking with great wine, concerts, working out and playing with her dogs.