Varus knees, also known as genu varum, occurs when the knees bend away from each other in a standing position. This can lead to foot supination, where the weight of your feet is shifted to the outer side. Sometimes varus knees are associated with a flattening of the low back curve.
Genu varum is normal in infants and toddlers under age two. After this stage, if it presents on one side or comes on suddenly, there may be an underlying problem that may require treatment.
Varus vs. valgus knee
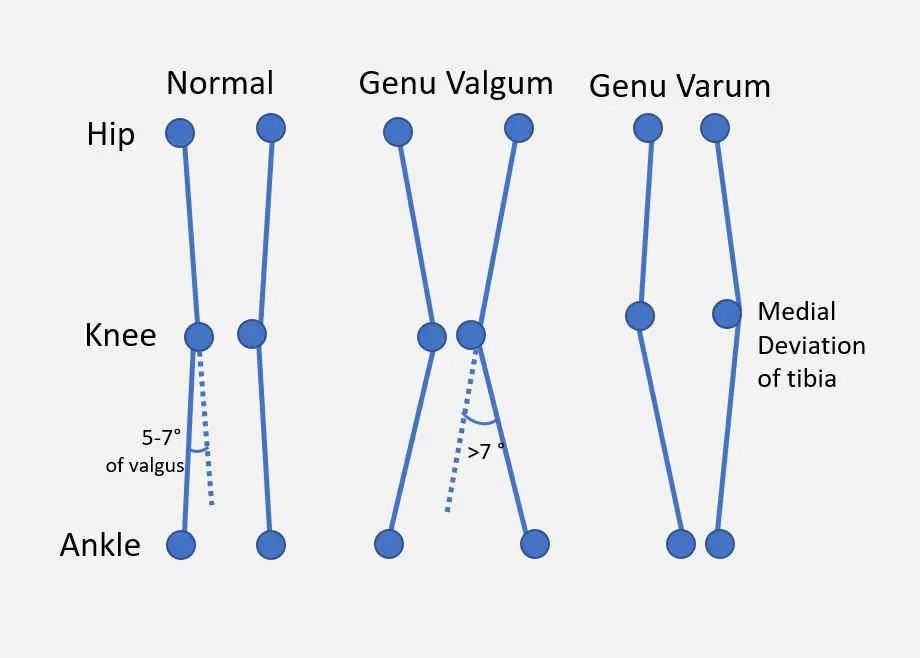
A simplified comparison of “normal,” valgus, and varus knees. (Image by Dr. Vijaya Chandar, licensed under the Creative Commons Attribution-Share Alike 4.0 International.)
In knee varus, the knees curve away from one another, even with the ankles touching in standing. This is also referred to as being ‘bow-legged’ (which refers to the curve of an archer’s bow) or ‘bandy-legged.’ Picture a classic cowboy stance, and that’s varus.
In valgus knee, the knees angle in towards one another and likely touch in a standing position. This causes the lower legs to splay out with the feet spaced apart. There may also be inward rotation of the tibia (shin bone) and rolling in of the ankles, known as foot pronation. This can contribute to an increased lordosis and anterior pelvic tilt.
The tibiofemoral angle, or TFA, is used to measure the angle between the axes of the femur (thighbone) and the tibia. Generally, ‘normal’ TFA is defined as being in the range of six degrees of valgus with women slightly higher than men on average. Anything more than 10 degrees of valgus or less than zero degrees is considered a malalignment—although there is variation in the scientific literature regarding measurement parameters and descriptions.
However, the TFA isn’t that accurate: it’s a two-dimensional measure of a mobile, three-dimensional structure, and its accuracy can be compromised by other variables, such as a curve in the femur.
Symptoms of varus knee
Common symptoms of varus knees are:
- bowing out of the knee with the ankles touching in a standing position;
- lower Q-angle;
- osteoarthritis at the medial aspect of the knee between the patella and femur;
- knee pain in the inner part of the knee;
- instability—feeling like your knee will “give out”;
- possible low back pain
Varus knee causes
Knee varus is often normal before age two, but if it persists after this age, it may be a symptom of an underlying disorder or pathology. Idiopathic knee varus occurs when the varus alignment persists past age two without another known cause.

Varus knees can be caused by nutritional deficiencies, such as rickets. (Image by Umeedhom, licensed under Creative Commons Attribution 3.0 Unported.)
Some of the causes of varus knees include:
- Nutrition deficiencies: this can affect bone growth and formation during a child’s growth. These include Blount disease, achondroplasia (a common cause of dwarfism), Paget’s disease, tumors, infections, or arthritis. Calcium and vitamin D deficiencies may lead to osteomalacia and rickets, which may cause varus.
- Injury
- Leg length discrepancy
- Ostearthritis
Varus knee treatments
There are some options for treatment of knee varus. The appropriate treatment several factors, including age, health and lifestyle history, and the degree of varus.
Orthotics
Orthotics are devices used to alter mechanics and redistribute force. They have been used in treatment of knee varus and valgus, such as laterally wedged foot orthotics as well as ‘valgus unloader’ knee braces, which may be used in conjunction with each other.
Valgus unloader braces are often used for the management of medial knee arthritis, frequently associated with varus knee alignment. They are designed to ‘open up’ the medial aspect of the knee joint during weight-bearing by inducing a force into the joint, transferring the load through the brace itself, and into the other side of the knee joint.
Valgus braces may affect mechanics and change load distribution during gait, however the effect may be so small as to be clinically irrelevant. This minimal mechanical effect does not appear to be associated with long-term improvement in pain and functional activity outcomes, although bracing may offer beneficial support in short-term rehab.
There’s very little quality evidence to inform recommendations regarding use of knee braces in varus arthritis, but the available evidence fails to support their use.
Lateral wedge orthotics aim to indirectly correct the angle at the knee by changing the position of the ankle. By raising up the outer side of the foot, the ankle may be brought out of supination, lessening external rotation of the tibia and associated varus knee positioning.
Although this seems to make sense, orthotics have not been found to provide long-term benefits to patients experiencing medial knee osteoarthritis. When compared to a neutral insole added to the shoe, they provide no additional benefit in pain or functional outcomes. There’s a lack of any quality research support for the use of these devices.
Exercise
Exercise can help reverse varus knee alignment with mild or no symptoms. The strengthening certain muscles and joints, it may “pull” your knees into better alignment.
Squat with adduction
This exercise strengthens your inner thigh muscles (adductors) and maintains knee alignment as you squat.
- Place a small foam roller, medicine ball, or a similar object between your knees. The object should be large enough to keep your knees and feet about hip-width apart and offers mild cushioning to your knees.
- Stand with your feet pointing forward or slightly outward.
- Inhale as you squat down as low as you can or at least until your buttocks move past your knee level.
- Exhale as you stand back up. Perform 8 to 10 reps for 2 to 3 sets.
- You may also do this exercise with a stability ball at your back, propped up against a wall.
Lunge with elastic band
This exercise uses the same concept at the squat with adduction but you’re working on one side of your lower body at a time.
- Secure an elastic band to a sturdy object like a heavy table or wall hook. Wrap the band around your right thigh near your patella so that the band pulls your knee away from your body’s midline. This forces you to pull your knee toward the middle of your body.
- Stand with your right foot in front of you and your left foot behind you. Your feet should be about 2 to 3 feet apart, depending on your leg length and height.
- Inhale as you lunge down until your left knee almost touches the floor. Keep your torso upright, but you may lean forward slightly. Your right knee should either match your toeline or move slightly beyond it.
- Exhale as you stand back up. Perform 8 to 10 reps for 2 to 3 sets per side.
Physical therapy
Physical therapy can help by using orthotics, braces, therapeutic exercise programs, and manual therapy. The goals of treatment will depend on the varus condition as well as patients’ goals.
In pediatric cases, exercises may be used with manual therapy to positively influence gait patterns and muscle development.
Physical therapists can also:
- support an active lifestyle and independent living
- assist in maintaining mobility and managing pain
- guided exercise programs
Also, manual therapy with exercise has some promise in the short-term management of painful knee arthritis and may contribute to short-term improvements in mobility. It may also lower sensitivity and pain responses in the short term. Pain is a complex phenomenon, involving both sensory input from the body and central nervous system perceptions and responses related to that input.
Surgery
In cases of severe or progressive varus knee misalignment in children, surgery can be a safe and effective approach. The goal of surgery is to control the final position of the joint by influencing growth prior to skeletal maturity.
An open- or closed-wedge osteotomy may be performed, which involves either inserting or removing a wedge of bone from the femur or tibia to affect the final position of the joint.
Another method used is hemi-epiphysiodesis, which is a technique used to stop bone growth on one side, either temporarily or permanently. This is used for correction of leg length discrepancy as well as valgus or varus deformities.
Sometimes hemi-epiphysiosesis is used to inhibit and guide growth, including stapling or surgical placement of a metal device attached across the growth plate. Patients may get total correction with relatively low complication rates using modern surgical techniques. When the desired alignment is achieved, the hardware is removed.
Surgery may also be considered for patients with severe arthritis associated with a varus alignment. Varying surgical approaches may have different levels of success, with some showing good long-term benefit and others only providing short-term improvement. These surgeries may also be performed with a goal of delaying or eliminating the need for an eventual total knee replacement.
In the most severe cases of osteoarthritis, a total knee replacement may be performed, and any valgus or varus malalignment will be corrected.

Frances Tregurtha, RMT
Frances has been a registered massage therapist in Ontario, Canada, since 2000, and she is working toward completion of a diploma in manual osteopathic practice.Her clinical background includes private practice, long-term care, and palliative work, as well as motor vehicle injury rehab and work with traumatic brain injury patients.
She currently works in two clinics, one of which is a multidisciplinary setting focusing on women’s health and pediatrics.
Outside of work, she can be found with her family and dog, cooking, gardening, camping, hiking, beach-going, and squeezing in a moment here and there for yoga and a scenic jog.