Pronation is a normal motion at the ankle joint where your foot and ankle rolls inward after making contact with the ground. This helps to absorb shock when you walk and run. It’s part of a normal gait pattern as you transition from midstance to your toes as you push off to the next step. While it is important, having too much pronation can cause some problems in your feet and ankles.
What is normal pronation?
Normal pronation is difficult to measure because it occurs around three planes of motion simultaneously. Some people describe “normal” as 15% of inward ankle rolling, but there’s no clear reference point and this number is not useful.
Instead of using percentage of motion, researchers have found that pronation can be measured by using a combination of other foot postures, including navicular drop, navicular angle, calcaneal eversion, Achilles angle, and longitudinal arch angle.

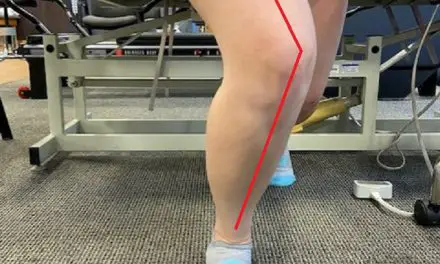
Normal foot pronation. (Photo by Penny Goldberg)
Foot posture is often classified as pes cavus (high arch/supinator) or pes planus (low arch/pronator). If your ankle often deviates from neutral foot posture, either from too much pronation or supination, it can develop structural and functional problems. Oftentimes, these biomechanical issues are seen in the joints and soft tissues above and below the problem area.
Does overpronation cause pain?
Overpronation has been linked to injuries in the lower body for as long as humans have been walking on two legs. This extra range of motion is thought to cause abnormal stress to the ankle and feet, as well as up to the knees, hips, and lower back.
Foot overpronation may cause:
- flat feet
- pain in the ankle, heel, calf, and/or Achilles tendon
- fallen foot arch
- plantar fasciitis
- bunions
- excessive callus and corns at the ball of the foot

Too much pronation may cause flat feet. (Photo by Penny Goldberg.)
Current research has found some evidence to support that overpronation of the foot can increase the risk of pain and injury.
- A 2011 systematic review reported that high-arch and low-arch foot postures are risk factors for developing running related injuries, including medial tibial stress syndrome and plantar fasciitis. A study of military recruits found those with an overpronation developed medial tibial stress syndrome more often than those with a neutral foot posture.
- A similar study found that in 25 female runners, those with a history of plantar fasciitis had a low arch or pronated foot posture, more often than age-matched controls. This suggests that identifying those who are excessive pronators before they start training may be beneficial in decreasing the incidence of medial tibial stress syndrome and plantar fasciitis.
Overpronation is related to increased knee flexion during dynamic movements. This theoretical model suggests that the relationship between knee flexion and overpronation can be explained, in part, by the increased internal rotation of the tibia that occurs with pronation.
And so, increased knee flexion has been associated with higher compression forces at the knee which could be a link to excessive pronation and patellofemoral pain syndrome (PFPS).
Another connection between pronation and knee pain may be the Q-angle, or quadriceps angle. It represents the angle of pull of the quadriceps and is both responsible for—and subject to—other forces in the lower body.
Too much time spent in hyperpronation creates increased internal rotation of the tibia which may lead to excessive medial knee stresses and lateralization of the patella from tight soft tissue structures. The combination of excessive Q-angle and overpronation may speed up the progression from knee pain to knee arthritis to degenerative joint disease or osteoarthritis.
Foot overpronation treatment
There are some treatments that may correct or reduce foot overpronation.
Pronation and orthotics
Orthotics provide support for the foot arch and is the easiest way to decrease stress and alter foot posture. They can be used to bridge the gap between the source of the dysfunction and interventions to address it, including stretching, strengthening, neuromuscular re-education, and massage.
Physical therapy
Research shows that physical therapy is an effective treatment to reduce overpronation and its symptoms. This includes a combination of exercise, manual therapy, taping, and other non-invasive methods
For instance, a study of 41 people with flat feet who did a six-week foot exercise program had a decreased drop in their navicular bone, enhanced foot posture, reduced foot pain and disability, and increased plantar pressures in the midfoot.
Another study on the effectiveness of a robust therapeutic exercise program among 58 teenagers with foot overpronation showed that all biomechanical parameters and gait improved with the 12-week program.
Change of shoes
Despite the popularity of high-arch shoes and minimalist shoes in the early 2010s, current evidence does not support much of using special shoes to address overpronation. It appears that an awareness of foot posture during the stance phase of running—specifically at the point of maximal pronation—may be more clinically useful than trying to match shoes to foot type.
For example, in 2010, Canadian researchers evaluated the efficacy and safety of suggesting motion control shoes to female runners. They found that those in motion control shoes had more injuries and more missed training days than those in stability or neutral shoes.
A similar study among military personnel found no difference in injury risk when shoe type was selected based on the shape of the foot compared to a group that used stability shoes regardless of foot shape.
More and more evidence suggests that training errors, not foot posture, may be the cause of up to 70% of all running injuries. Runners may be more well served to focus on training guidance instead of foot posture and shoe selection.
Foot pronation and massage therapy
As with every condition, it’s important that massage therapists perform a thorough evaluation and understand where and when their client is experiencing pain and dysfunction. Simply observing their anatomy and finding a pronated foot does not mean a pathological issue is present. The key challenge for massage therapists is to determine at what point these imperfect mechanics are leading to soft tissue pain or injury.
However, you can use massage therapy as an adjunct treatment of overpronation, but it’s important that the therapist understands how the tissues are being affected so that they can choose appropriate techniques. In overpronation, the tibialis posterior is not eccentrically resisting pronation like it should be, but the muscle is unlikely to be short or contracted. More likely, it’s being overstretched by the collapse of the medial arch.
Massage techniques targeting posterior tibialis should focus on decreasing hypertonicity rather than increasing extensibility. Tibialis posterior is most effectively treated side-lying with the affected side on the table so that the medial aspect of the leg is accessible.
If active stripping techniques are being implemented, it may be necessary to apply manual resistance through the plantar surface of the foot to elicit an appropriate level of contraction for the technique to be effective. Working in this region can be quite painful, so be sure to check with your client often regarding tolerance and proceed with caution.

Penny Goldberg, DPT, ATC
Penny Goldberg, DPT, ATC earned her doctorate in Physical Therapy from the University of Saint Augustine and completed a credentialed sports residency at the University of Florida. She is a Board Certified Clinical Specialist in Sports Physical Therapy.
Penny holds a B.S. in Kinesiology and a M.A. in Physical Education from San Diego State University. She has served as an Athletic Trainer at USD, CSUN, and Butler University.
She has presented on Kinesiophobia and differential diagnosis in complicated cases. Penny has published on returning to sports after ACL reconstruction and fear of movement and re-injury.
Outside of the clinic, Penny enjoys traveling, good cooking with great wine, concerts, working out and playing with her dogs.