Scleroderma, named from the Greek roots σκληρός (skleros, “hard”) + δέρμα (derma, “skin”) is an autoimmune disorder. It’s considered a rare disease because in samples of 1 million Americans, you would expect to find about 250 of them—about 0.025%—living with scleroderma.
Out of five people who have scleroderma, four of them will be women. While it usually occurs in adulthood, children have been known to contract it, too. Scleroderma has been researched in mice because they also get a form of the disease.
Scleroderma is related to other autoimmune and connective tissue diseases, such as rheumatoid arthritis, Sjögren syndrome, lupus (usually referring to systemic lupus erythematosus or SLE), EDS, and multiple sclerosis. These diseases are related because they all result when someone’s immune system responds abnormally to a possible threat.
The immune system attacks the body’s healthy tissues as if they are pathogens themselves. What makes the diseases different from one another is what body parts each one tends to affect.
For example, rheumatoid arthritis tends to affect joints (especially fingers and wrists), Sjögren syndrome tends to affect moisture-producing membranes, such as eyes, mouths, and vaginas, and contribute to inflammatory bowel disease that tends to affect colons and small intestines.
But immune systems and connective tissues are particularly complex areas of health and illness, and the conditions described under the umbrella term “autoimmune diseases” do not always conform to their descriptions.
Overlap syndromes, such as mixed connective tissue disease, have symptoms that resemble other autoimmune conditions, such as scleroderma, lupus, and rheumatoid arthritis. Whole-body diseases (e.g. lupus) attack entire systems—unlike type I diabetes, which primarily attacks only the pancreas.
When you take into account how these conditions can overlap, complicate entire body systems, and how rare some of them are, you can see how complex the clinical picture for many autoimmune conditions can be.
Massage and other manual therapists do not need to be experts on whether “mixed connective tissue disease” and “undifferentiated connective disease” are the same or not. Even medical doctors aren’t experts in discussions like that, and therapists don’t have to be either.
Their job is this: to be there for their clients or patients. They should know enough about the conditions so that they can provide safe and effective care.
They need to have enough security and humility to be able to update their knowledge as new and validated information becomes available. And they need to be able to listen to their clients or patients with their whole hearts
People who have scleroderma can benefit much from massage therapy, and therapists have a lot to offer them.
What are scleroderma symptoms?
There are several different kinds of scleroderma, so the signs and symptoms can be very different from one person to another, and they may or may not be apparent to other people. Skin signs and symptoms like the following are the ones we are most likely to see in the clinic.
These pictures show different kinds of effects that scleroderma can have on skin. What you are seeing here is the back of a person living with scleroderma.

Photo: “MercMorphea” by Leith C Jones is licensed under CC BY 3.0.
Scleroderma can also cause stiffness and darkening of the skin.

Photo: “Left Arm Scleroderma Patient” by AVM is licensed under CC BY 3.0.
This person’s finger joints directly beneath their nails are noticeably darker and shinier than the rest of their hands.
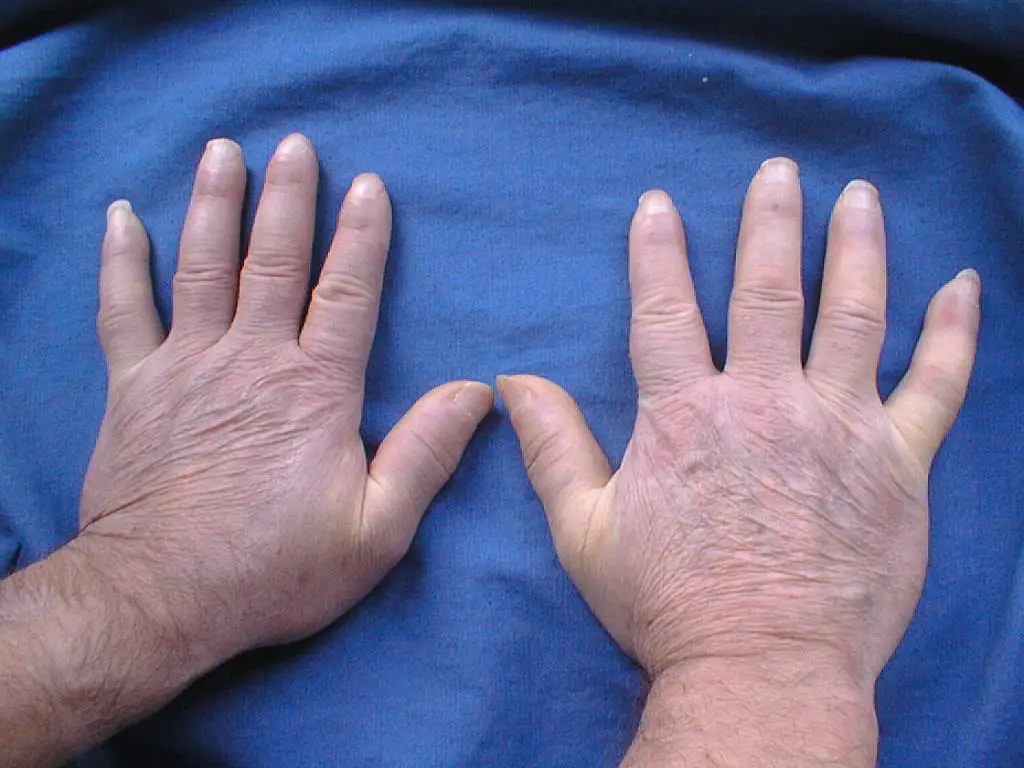
Photo: “Systemic sclerosis, changes on hands are allways bilateral.jpg” by Maria Sieglinda von Nudeldorf is licensed under CC BY-SA 4.0.
Some clients may experience Raynaud syndrome as well.

Photo: “Raynaud’s Syndrome.jpg” by Tcal is licensed under CC BY-SA 3.0.
People may also live with musculoskeletal and joint pain or weakness, often on both sides of their body. Range of motion can be affected or limited by skin, muscle, or joint involvement. Many people living with scleroderma experience contractures of joints such as their fingers.
Manual therapists treat all of these signs and symptoms as they would treat them for anyone else not living with scleroderma. This includes observing the best standard practices around indications (e.g. pain in intact skin and muscles) and contraindications (e.g. pitting ulcers).
If massage therapists come across a sign or symptom that they do not understand, then they should leave it out of the massage until they can find out more to understand what is going on, and whether and how to treat it.

Photo: “Systemic sclerosis finger.jpg” by Frank Breuckmann, Thilo Gambichler, Peter Altmeyer and Alexander Kreuter is licensed under CC BY 2.0.
In addition to skin issues, scleroderma can cause digestive symptoms such as gastric reflux or diarrhea.
Chronic digestive problems can be exhausting and demoralizing to live with because eating is such an integral part of our lives and of socializing with other people.
What causes scleroderma?
A good deal of research into scleroderma is intended to better understand what causes scleroderma in some people and not in others.
Our current best understanding of what causes scleroderma is that it’s a combination of genes that some people are born with (and that others do not have) and the environment that they live in.
Changes in genes cause them to produce proteins that have certain effects, and multiple genes are probably involved in the body changes that scleroderma causes. There’s no particular reason why someone is born with such a genetic change—it’s just a thing that happens sometimes.
While there are a few cases of one gene inevitably causing one disease with no escape from it (the Huntington disease that killed the American folk singer Woody Guthrie is a good example), that kind of direct cause-and-effect at the genetic level is relatively rare.
Much more common is a situation where someone is born with genes that have the potential to cause a disease. Then—depending on what is in their environment that may or may not turn on those genes—sometimes the gene may turn on and trigger that disease.
In other people, the gene may never turn on. While the potential always remains there, the disease never actually develops. Why this happens sometimes in some people and not in others is an active area of research into the causes of scleroderma.
What is CREST syndrome?
CREST syndrome, named for five of its main symptoms, is sometimes called a “limited” form of scleroderma because it’s not as widely systemic as the primary form of the condition.
CREST stands for:
- Calcinosis
- Raynaud syndrome
- Esophageal dysmotility
- Sclerodactyly
- Telangiectasia
It’s important to remember, though, that “limited” refers only to the extent of the syndrome—it does not mean that CREST is not potentially dangerous.
It also doesn’t mean that the illness burden is easy for clients to live with. CREST can cause serious pain, and it can also lead to life-threatening complications, such as lung involvement or heart failure, and clients can experience problems as a result of living with CREST.
It’s crucial to listen to what clients tell you about their experiences, and to do what you can with massage—modifying it, if necessary, based on what signs and symptoms the client is living with—to offer relief and therapeutic support.
Remember, though, that people are different from each other, and that autoimmune conditions can vary widely. CREST, like other autoimmune conditions, can be hard to diagnose, and the ambiguity of not knowing exactly what is wrong can add to the client’s illness burden.
The symptoms can be treated, but—like the more extensive and systemic scleroderma—there is no cure for CREST syndrome. Like other autoimmune conditions, CREST is also not contagious—you can’t catch CREST from massaging a client.
Calcinosis. People living with CREST often experience the deposit of calcium compounds in their skin. Although there are medications for calcinosis, it is not an easy condition to treat.
Massage therapists can be supportive of calcinosis treatments by avoiding deep pressure, keeping treatment rooms comfortably warm and providing extra linens to the client’s comfort, and helping provide stress reduction.
Raynaud syndrome. Raynaud syndrome is a condition in which spasms in small blood vessels in fingers and toes cause those blood vessels to cut down on blood flow in those areas, often causing cold sensations and pain.
There are multiple causes and triggers for Raynaud syndrome, including stress and cold temperatures, so having the syndrome does not in itself mean that a person is living with CREST. But Raynaud syndrome is one of the symptoms that provides CREST with its name, and it can have a large effect on the quality of life of clients living with CREST syndrome.
Massage therapists can be supportive of clients living with Raynaud syndrome by treating involved areas as a local contraindication during an acute attack, and providing gentle massage in those areas when the client is not experiencing blood vessel spasms.
Esophageal dysmotility. Clients living with CREST syndrome can experience the feeling of having food “stuck” and unable to move properly through the esophagus, due to CREST’s interference with its motility.
There are a number of ways that massage therapists can be supportive of clients living with esophageal dysmotility.
If the client complains of it as a new symptom, encourage them to check it out with their primary healthcare provider, if they haven’t done so already.
Providing different positioning options, such as sitting rather than lying supine, may be somewhat helpful, but if they’re having an attack during their massage session, it’s better to reschedule the massage for another time.
If you plan to make a career working with clients with complex medical histories, you may want to structure your practice so that you can support a generous rescheduling policy for those clients, as complications like esophageal dysmotility can occur with little or no warning.
Sclerodactyly. Named from the Greek roots σκληρός (skleros, “hard”) + δάκτυλος (daktulos, “finger, digit, fingers and toes”), sclerodactyly means “hard fingers/toes”, and gets its name from the hardening and tightening of the skin on the fingers and toes that clients living with CREST may experience.
Sclerodactyly is an indication of tissue damage, so avoid deep massage to hands and feet, and if it has progressed to ulceration, then avoid the areas entirely, focusing your massage on areas that are not undergoing obvious tissue damage.
Telangiectasia. Named from the Greek and Latin roots τέλος (telos, “end”) + ἀγγεῖον (angeion, “blood vessel”) + ἔκτασις (ektasis, “stretch”), telangiectasia refers to small clusters of dilated capillaries, sometimes also called “spider veins”.
If your client living with CREST experiences telangiectasia in their legs, you can be supportive by providing bolsters to keep their legs elevated during the massage. Don’t perform massage directly on an area with telangiectasia, although an extremely soft gliding stroke to transition to another area is probably safe.
Your client is the expert on what the experience of living with CREST is like for them. Ask open-ended questions, communicating that you are genuinely interested in their answers, and look for ways that your massage (with or without creative modifications) can be supportive in providing a better experience, whether in timing, choice of stroking, positioning, depth, or other aspects of the massage.
“If you saw me, but didn’t look at my hands, you would say I look good. But people with chronic pain hate to hear that—it’s like an old, old book with a good jacket, but inside are tattered pages, bent corners, scribbled on with crayon, missing pages.”
Massage and scleroderma: what can it do?

“If you saw me, but didn’t look at my hands, you would say I look good, but people with chronic pain hate to hear that.” Photo courtesy of Choice Kinchen.
If you understand how genes and environment together can sometimes trigger the expression of scleroderma, and if you can provide a safe and supportive environment for people to express their own experiences and feelings around being one of the people in whom the disease is taking place, then massage therapy can provide an extremely valuable service to you.
Choice Kinchen, LMT, who practices in the greater Austin-Pflugerville area in Texas, has a particularly well-informed and integrative view on massage and scleroderma while living with adult-onset scleroderma.
“If you saw me, but didn’t look at my hands, you would say I look good,” Kinchen said, “but people with chronic pain hate to hear that—it’s like an old, old book with a good jacket, but inside are tattered pages, bent corners, scribbled on with crayon, missing pages.”
If we talk to our clients who are living with chronic conditions like scleroderma only about what we see, then we’re sending a message that we’re not listening to what they are saying about what things are like for them. They may even shut down.
Even though we might intend to be encouraging, such a statement can block communication, rather than promoting it. Many people with chronic conditions are used to having to censor their true speech because the reactions from other people can be exhausting.
Instead, we have the potential to provide a safe and welcoming space for them to speak honestly about what is going on with them—and not to have to hide it or to sugarcoat it in order to protect our feelings or fears. That is a value that people living with chronic conditions can treasure.
[Related story: Why Massage Therapists Should Understand How Pain Works]

“Never tell me I can’t do something. I just haven’t tried it yet, and I’m going to give it my best shot,” said Choice Kinchen, LMT, who works at First Choice Massage in Pflugerville, Texas. Photo courtesy of Choice Kinchen
The way that massage therapists communicate that they are genuinely interested in what’s going on for them is to ask rather than to tell. Ask genuinely how they are doing, and be prepared to follow where the answer takes you.
Kinchen mentioned that his hands display visible signs of his scleroderma. Since his hands help make his living, that raises the question of how he can perform massage therapy.
He was told that he could not, but he has proven his critics wrong. He had to make modifications to his techniques to work around what his hands can and cannot do.
Gliding does not work for him and he can’t feel with his elbow, but he says that he can make a soft fist instead; he can use his knuckles, he can grasp the client’s fingers and neck in a chair massage, and he uses leverage to deliver appropriate force and direction.
In 21 years of practicing massage, Kinchen has learned the tricks of the trade and ways to approach different people with different presentations.
“Never tell me I can’t do something,” he says. “I just haven’t tried it yet, and I’m going to give it my best shot.”
In turn, massage therapy has benefited him by keeping his joints moving, keeping his hands in good shape, and possibly delaying contractures in his fingers and hands. While he does not believe that massage can totally prevent contractures, he does credit it with possibly slowing their progression by keeping his joints moving, keeping his hands in good shape, and making them less vulnerable to curling up and contracting.
In his practice and in his daily life, Kinchen is conscientious about practicing infection control. Because it is an autoimmune disease, treatments for scleroderma often involve immunosuppressant drugs, which can leave people living with scleroderma highly vulnerable to any infection in their environment.
“If my grandkids are sick, then I don’t go around them—sometimes I just have to walk away. It’s very hard because they don’t understand why I have to do it,” he explained.
What can massage therapists do for clients living with scleroderma?

You’re not expected to be experts on scleroderma, but you should know enough about the condition to ask appropriate questions on the intake form. Photo courtesy of Choice Kinchen
As aspiring healthcare professionals, you can support and empower your clients in the following ways:
- Understand that clients with “invisible diseases” like scleroderma often will take on the burden of protecting you and your feelings if they sense that you are distressed by the reality of their experiences. If you minimize (“That’s not so bad”) or you make it about yourselves (“You look good to me!”)—even if you intend to be encouraging—you can have the opposite effect.The client can shut down and start offering only superficial answers (“I’m fine, and yourself?”).
- Take that burden off your client by asking inviting questions about their experience and feelings, and really listening to their answers. If a client’s response opens the door to more questions, then follow them with genuine interest.
- Ensure that you are able to shoulder this healthcare professional burden by having a good support system outside of work, and practicing regular healthy self-care. You, too, have needs that you have to ensure get met, but you have to do so from people who are not our clients, so that you can provide a safe environment for them.
- You’re not expected to be experts in scleroderma, but you should know enough about the condition to ask appropriate questions on the intake form, what effects any medications they’re taking may have on their ability to receive a massage, on indications and contraindications, and any further massage questions that may be involved.Just as you’re the experts on massage, the person living with scleroderma is the expert on what that experience is like. We need to ask them what works for them, and we need to listen to their answers.
- In addition to asking about experiences and feelings, ask about practical things you can do. For example, all someone wants is a cup of coffee.
- Be prepared to make adjustments to your massage routine if necessary to work with symptoms the client may have.
- Follow standard indications and contraindications as you would for any other client.
- Understand the constraints that the client’s condition may cause them, but don’t treat them as though they are sick, broken, or fragile.
Kinchen once bicycled 1,350 miles from Houston, Texas., to Dearborn, Mich., to raise awareness of scleroderma, an amazing feat of endurance for anyone in any condition. Let the client tell you where they are, and be ready to meet them there. - Provide a safe and respectful place for the client to receive a massage. One client reports a harrowing story in “Asking for a Massage, and Getting a Sad Lesson in Prejudice.” Don’t be like the massage therapist in that story. Instead, be knowledgeable, prepared, kind, and professional.