If you’re struggling with arthritis pain, you may find relief with massage therapy. The benefits of massage include improved local circulation, relaxation, and pain reduction. It is not a cure for arthritis, but it can allow you to move better and live more independently. This article examines how massage works and the scientific evidence behind its effectiveness for arthritis.
What type of massage is best for arthritis?
Massage that focuses on gentle techniques can be effective in the management of arthritis.
Some types of massage that can be used include:
- Swedish massage: Uses light to medium pressure through long, gentle strokes to improve circulation and relaxation.
- Myofascial release (MFR): Reduces stiffness and improves mobility in affected areas through targeting the connective tissue that supports the joints.
- Lymphatic drainage massage: An extremely gentle technique that helps reduce swelling and inflammation by enhancing the flow of lymphatic fluid.
- Trigger point therapy: A more aggressive technique that may be used when the muscles that surround the joint are tight. It should only be used if it doesn’t increase joint pain.
While research on the impact of specific massage techniques for arthritis is limited, experienced massage therapists can often identify the techniques they’ve found to be most effective for a particular patient. The therapist’s choice of technique is primarily guided by the desired outcome, such as relaxation, rather than the specific body part being treated. However, there’s some consensus about which joints and muscles respond best to specific techniques.
In general, the tissues surrounding the neck and shoulders respond favorably to Swedish massage and MFR. Because many people tend to hold tension and stress in these areas, gentle strokes that loosen muscles, increase circulation, and reduce tension can be beneficial.
The smaller joints of the hands, wrists, feet, and ankles can suffer some of the most severe arthritic changes. These joints often benefit from lymphatic drainage and trigger point therapy applied to the muscles of the hand and forearm. Similarly, lymphatic drainage and reflexology may be effective in reducing pain and improving function in the feet and ankles.
The larger joints of the lower body, specifically the hips and knees, can generally tolerate deeper massage techniques. Consequently, these areas may be best addressed with deep tissue massage to target muscle tightness, in conjunction with Swedish massage and MFR.
How does massage work for arthritic pain?
There are several mechanisms by which massage can help in the management of arthritic pain.
Descending modulation
Descending modulation is like your brain’s built-in pain control system, where your brain can turn the volume up or down on nociceptive signals traveling through your nervous system. Nociceptive signals are messages sent by special sensors in our body called nociceptors when they detect something that might hurt us. Nociceptors can detect extreme heat, pressure, harmful chemicals, and other things that may be harmful to you. When they sense danger, they send electrical signals through your nerves to our spinal cord and brain.
However, these signals aren’t the same as pain. Pain is what you actually feel and experience. It’s more complicated than just the signals themselves because pain involves our emotions and cognition, which affect how your brain interprets these signals.
Imagine your brain as a control room that can send messages down your spinal cord to either reduce pain (like when you’re in an intense situation and don’t feel pain) or sometimes increase pain sensitivity. During a massage, gentle pressure and movement can be used to stimulate mechanoreceptors in the skin and muscles. These sensations of light touch and movement are transmitted to the brain and activate the descending inhibitory pathways and reduce pain perception.
Also, massage can release natural pain relievers, such as endorphins that inhibit or reduce nociceptive signals in the spinal cord.
Gate control theory
Gate control theory of pain posits that non-painful stimuli can interfere with nociceptive signals in the spinal cord, effectively “closing the gate” and reducing pain perception in the brain.
Most of us use this theory of pain modulation without even thinking about it. A commonly used example is hitting your thumb with a hammer. When the pain is felt, our natural instinct is to shake our hand. This non-painful stimulation (the shaking) will “close the gate” to the nervous system so that the nociceptive signals can’t be transmitted. Massage can also close the gate.
Biopsychosocial (BPS) model
The holistic approach to care offered by massage therapy fits well in the BPS model of pain. Massage doesn’t just treat the signs and symptoms of arthritis; it addresses the whole person. The effects of massage can be seen in the biological, psychological, and social dimensions.
Biological
- Decreased muscle tension, improved circulation, descending pain pathways
- Increased release of endorphins and serotonin
- Decreased inflammation, improved lymphatic draining, and improved tissue mobility
Psychological
- Stress reduction, lower cortisone levels and increased dopamine and serotonin
- Improved sleep quality and emotional regulation
- Encourages mindfulness and mind-body connection
- Reduced emotion intensity of pain via a calm nervous system
Social
- Therapeutic alliance between the therapist and client
- Therapeutic touch to promise a sense of care and attention
In a 2017 study published in Pain Medicine, researchers reported that patients with knee osteoarthritis who received regular massage had improved quality of life. This qualitative study also found that patients felt empowered to perform activities of daily living after having massage therapy.
Also, a 2021 systematic review and meta-analysis in Complementary Therapies in Clinical Practice found that massage improved functional outcomes in patients with osteoarthritis. More than 700 participants were included in these results that found a significant reduction in pain and stiffness after one to four weeks of massage therapy After six to eight weeks, there was a reduction in stiffness and functionality.
What should you expect from your first massage session?
Massage therapy clinics often have a soothing environment. The room will likely have dim lighting and soft music to promote a calming atmosphere. You will be instructed to undress to your comfort level. A licensed massage therapist will likely tell you if they want you to start face up or face down. Then they leave the room to allow you to prepare for your session to start.
The therapist should be very communicative. They should inquire about medical history as well as your specific diagnosis and symptoms. They may also ask about your expectations or goals for the massage which may include pain relief, improved mobility, stress reduction, or general relaxation.
Once the work begins, the therapist may ask often about pressure levels and comfort. If you need more or less pressure, they welcome your feedback.
The massage therapist will use a variety of techniques based on the interaction of your symptoms and what they feel. They will use broad, light strokes to make you feel comfortable and promote relaxation before moving to deeper, targeted techniques to address tight muscles. Sometimes it may seem like they are working away from the painful joints but this can be necessary to avoid aggravating any inflammation that may be present.
In terms of arthritis, different types of the disease may require different treatments or precautions:
- Osteoarthritis (OA): Responds well to gentle techniques that improve circulation, reduce stiffness, and increase range of motion. The therapist should be cautious with deep pressure on inflamed joints as this can worsen symptoms.
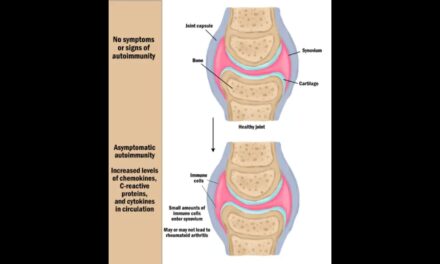
- Rheumatoid arthritis (RA): During flare ups, the therapist should take extra care to avoid increasing symptoms or range of motion. Sessions should focus on relaxation and light-touch techniques.
- Psoriatic arthritis: Consider skin sensitivity and avoid irritating any psoriatic plaques.
- Gout: Massage may not be appropriate during acute episodes but can be beneficial between flare-ups for circulation and joint health.
After the session, the therapist will discuss their observations and suggest follow-up care.
What should you do after a massage?
Once you’ve had a massage, the work is not done. The benefits of massage will last longer and be more effective if you participate in follow-up care.
Low-intensity movement such as walking, stretching, or yoga can boost the effects of the massage by increasing circulation and maintaining flexibility.
Other self-care activities that your massage therapist may want you to participate in could include: meditation, breath work, or self-massage. Or it could simply be getting a good night’s sleep.

Penny Goldberg, DPT, ATC
Penny Goldberg, DPT, ATC earned her doctorate in Physical Therapy from the University of Saint Augustine and completed a credentialed sports residency at the University of Florida. She is a Board Certified Clinical Specialist in Sports Physical Therapy.
Penny holds a B.S. in Kinesiology and a M.A. in Physical Education from San Diego State University. She has served as an Athletic Trainer at USD, CSUN, and Butler University.
She has presented on Kinesiophobia and differential diagnosis in complicated cases. Penny has published on returning to sports after ACL reconstruction and fear of movement and re-injury.
Outside of the clinic, Penny enjoys traveling, good cooking with great wine, concerts, working out and playing with her dogs.