Rheumatoid arthritis — or RA — is an autoimmune disorder that lasts a lifetime. It typically affects your joints, like fingers, shoulders, and knees, but it may affect your eyes, lungs, blood vessels, skin, and heart. Since massage therapy can help alleviate pain for many types of chronic pain conditions, it may also help your rheumatoid arthritic symptoms.
Whether arthritis is a disease or a disorder is debatable. Arthritis.org states that the term is an “informal way of referring to joint pain or joint disease.” However, some scientists say that it’s a “chronic inflammatory autoimmune disease” that is influenced by genetic, epigenetic, and environmental factors.
Rheumatoid arthritis is categorized as a type of undifferentiated connective tissue disease. This means the disease has signs and symptoms of one or more connective tissue diseases, which his makes diagnosis and treatments tricky and risky.
Because it’s an autoimmune disorder like scleroderma, EDS, and lupus (SLE), your immune cells attack your healthy connective tissues in rheumatoid arthritis.
While there’s no cure, there are treatments that can manage your symptoms to stop or slow its progression.
Causes
Research shows that some factors can increase your likelihood of getting rheumatoid arthritis.
Basically, your immune cells get into your joints and their connective tissues from your blood vessels. They “attack” your tissues, causing inflammation and swelling of your joints, which can be painful and warm to the touch.
One type of antibody called ACPA (anti-citrullinated protein antibodies) has been found to be a highly predictive indicator to having rheumatoid arthritis.
Genetics
A change in one or a few genes in some types cell-communication proteins—called cytokines—has been linked to developing rheumatoid arthritis. Whether this change occurs in one gene (“SNP”) or to a gene expression without changing the DNA sequence (“methylation”), both have been shown to increase the risk of getting rheumatoid arthritis.
Environmental
Smoking has been shown repeatedly in research to be a significant factor in developing rheumatoid arthritis, even among children. In fact, a 2021 longitudinal study of more than 90,000 female nurses, ages of 35 to 52, were asked a questionnaire about their condition every two years from 1989 to 2017.
While the researchers found “no significant” association between rheumatoid arthritis risk with maternal smoking during pregnancy or living with smokers after age 18, they found that persistent childhood exposure to cigarette smoking from parents is a significant factor in developing rheumatoid arthritis.
Other environmental factors include:
Organic and inorganic dust: A large Swedish study of more than 12,500 cases of rheumatoid arthritis with matching more than 129,000 controls found that exposure to textile and animal dust “are associated with increased risk of RA” provided that there is further evidence that the airborne exposures are a major cause of rheumatoid arthritis.
Damage and/or inflammation of the various lung tissues due to asthma is tied to cigarette smoke exposure and air pollutants.
Viral infections of the lungs: A South Korean study of more than 24,000 people with rheumatoid arthritis found that those who were exposed to the coronavirus (not COVID-19), parainfluenza, and metapneumovirus had increased the flare ups and other symptoms of rheumatoid arthritis. However, the researchers repoted that this is by no means proof of a cause-and-effect relationship.
Overweightness and obesity has been shown to increase certain gene expressions that contribute to joint inflammation.
First signs of rheumatoid arthritis
Early signs of rheumatoid arthritis include:
- Pain, stiffness, and/or achiness in more than one joint
- Swelling and tenderness in more than one joint
- Such symptoms almost always occur symmetrically in your body
- Fever
- Extreme fatigue
- Weight loss
- Weakness
Sometimes the symptoms can be mistaken for other conditions. For Eileen Davidson, who is a Canadian advocate for rheumatoid arthritis patients (Arthritis Research Canada), she had spent most of her twenties thinking that her chronic joint pain in her hands were from carpal tunnel syndrome.
Before she had the early symptoms of rheumatoid arthritis, Davidson was working as an esthetician in Vancouver, B.C., in her early twenties.
After many years of working in pedicures, massages, and facials, her hands, shoulders, neck, and feet hurt a lot, Davidson said. It wasn’t the typical aches and pains that go away after rest; her pain stubbornly persisted and sometimes flared up.
“I expected to go back to my job, but whenever I tried to get healthier like exercise or trying to work, I noticed those symptoms were still there but they were way worse.” (Photo courtesy of Eileen Davidson)
“From age 24 to 26, my job was getting more difficult and the pain was increasing,” she said. “I didn’t really understand why, and I was also getting sick a lot. I’m catching colds and flus, and it took me a long time to get rid of them.”
When Davison was pregnant with her son at age 26, she struggled with the same symptoms and still didn’t know she had rheumatoid arthritis.
“During my pregnancy, I didn’t feel any better,” she said. “A lot of women say they’d feel better during pregnancy, but I definitely didn’t. After my pregnancy, I expected a lot of the symptoms to go away — like my swollen feet and hands and depression.
“I expected to go back to my job, but whenever I tried to get healthier like exercise or trying to work, I noticed those symptoms were still there but they were way worse.”
Davidson had spent the next three years working as an esthetician despite having severe pain and fatigue until she was diagnosed with rheumatoid arthritis at age 29.
Is massage good for rheumatoid arthritis?
Many people with rheumatoid arthritis may find massage therapy can provide relief, but scientific evidence does not find a strong support for massage.
While a 2017 systematic review (based on seven studies with a total of 352 patients) found that massage therapy is “superior to nonactive therapies in reducing [arthritic] pain and improving certain functional outcomes,” the quality of the studies are low to moderate.
This means that some of these studies have a high risk of bias that likely favors massage over other treatments.
The authors concluded that there needs to be larger sample populations and more rigorous methods in future studies of massage for rheumatoid arthritis.
A 2023 systematic review of 13 clinical patient guidelines found that most non-pharmacological treatments, such as massage therapy and other manual therapies, have “no consensus” of recommendations for rheumatoid arthritis patients.
Paul Koziolek, who is a registered massage therapist for 15 years in Toronto, Ontario, at B Street RMT, said that most patients with rheumatoid arthritis have “muscle guarding,” where muscles spasm and try to immobilize the injured or painful area to prevent further injury.
“This is an automatic response to bone breaks and ligament, tendon or muscle tears,” Koziolek said. “For those with other injuries or disease processes, this can also occur to a lesser extent because of pain responses. I try to relieve this to the point where the patient has reasonable mobility and functionality for activities of daily living.”

“We cannot claim to heal these ailments, only provide non invasive relief.” ~ Paul Koziolek, RMT. (Photo courtesy of Paul Koziolek)
Massage therapy cannot cure or get rid of arthritic pain for good, but many people with arthritis may find some pain relief with massage.
While there isn’t much quality research in massage therapy for rheumatoid arthritis, the basic ideas behind how pain works can help answer how massage could alleviate pain — temporarily.
Descending modulation refers to the changes in parts of the brain that processes nociception (stimuli that signal actual or potential threat to you). These changes can pump up the pain “volume” up or down.
Therefore, different stimuli and the degrees of the stimuli would vary among different people. For example, a healthy person who bumps their hand against a table might not perceive the incident as a threat compared to someone with rheumatoid arthritis.
“However, we need to remember to operate within the bounds of our scope of practice,” Koziolek said. “We cannot claim to heal these ailments, only provide non invasive relief.”
What are the 4 stages of rheumatoid arthritis?
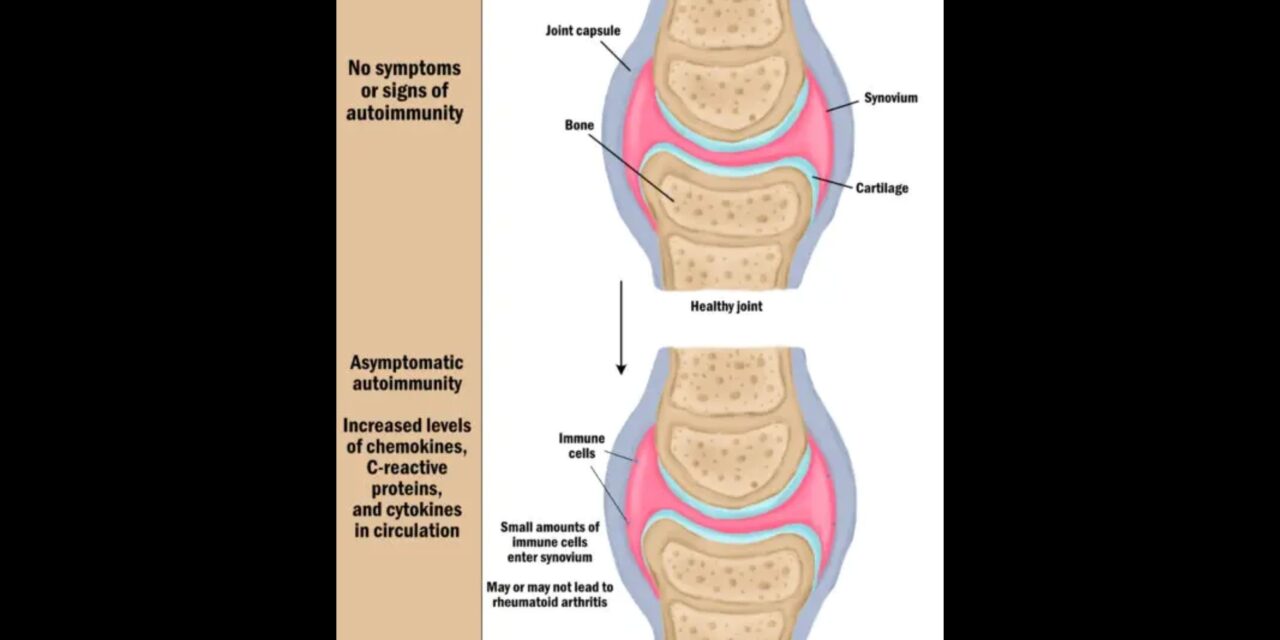
Research finds that rheumatoid arthritis undergoes four stages of progression. A group of Australian researchers highlighted the stages as:
Triggering stage: Stage 1 is where your immune cells attack your joints’ connective tissues, triggered by genetic and environmental factors. Your bone tissues aren’t affected yet.
Early symptoms include joint stiffness—particularly in the morning—and mild swelling of your joints. This stage is often too early for clinicians to determine whether you actually have arthritis or something else; thus, this is called “unclassified arthritis.” This term may also be used at the next stage.
Maturation stage: At stage 2, your body makes more antibodies from your bone marrow and lymph tissues, which causes more swelling and pain in your joints. ACPA levels are high enough to be detected in blood tests.
At this stage, the swelling, rheumatoid nodules, and other symptoms will likely come and go for several years before rheumatoid arthritis sets in your joints. Cartilages and other connective tissues are gradually degraded.
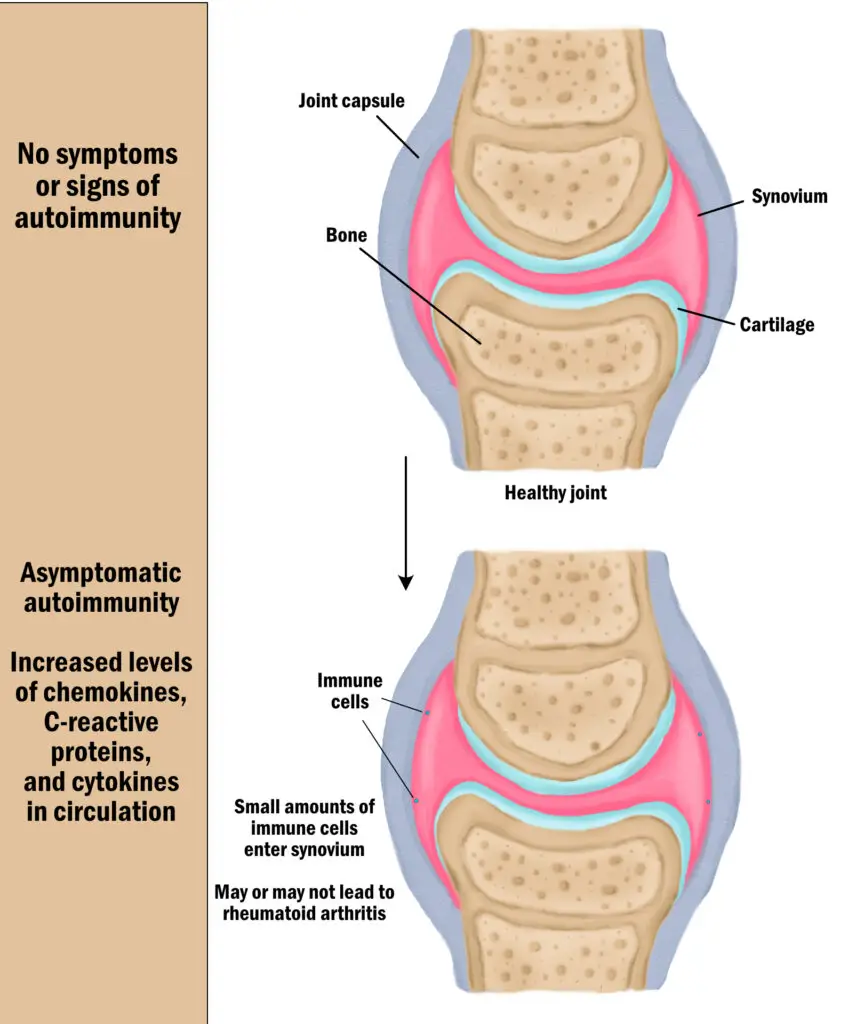
Rheumatoid arthritis is caused by a mix of genetic and non-genetic factors, and several of these factors need to build up before the disease begins. Rheumatoid arthritis starts when the immune system attacks altered proteins in the body, which can happen years before noticeable joint inflammation (synovitis) or symptoms appear. (Illustration by Nick Ng)
Key markers of rheumatoid arthritis include ACPA (anti-citrullinated protein antibodies), CRP (C-reactive protein), and RF (rheumatoid factor). (Illustration by Nick Ng)
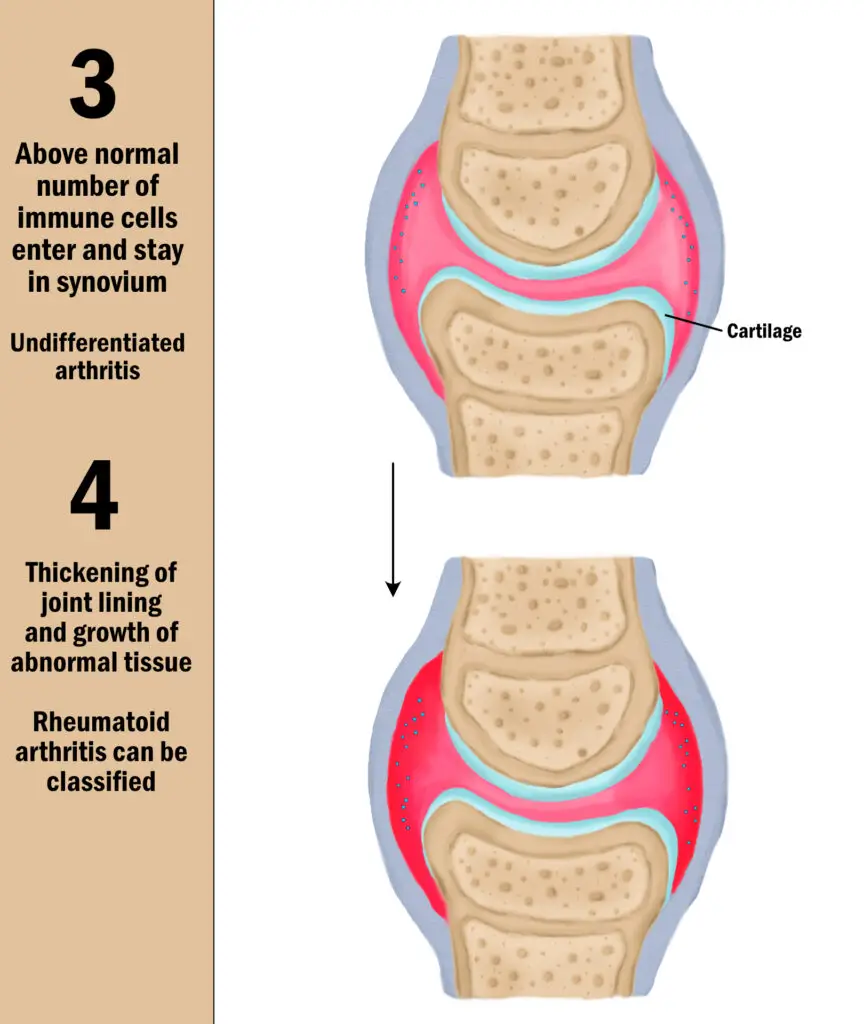
Targeting stage: The symptoms at stage 3 are more visible in your hands, fingers, and other joints. Symptoms of the finger and foot joints are often bent and crooked with limited movement. Sometimes the nerves in the joints pinches, which may cause pain.
The bursae and tendon sheaths are degrading to the point where the joints will be bone-on-bone contact.
On a cellular level, research has shown that there’s a huge amount of immune cells (macrophages) in synovial membranes, and an imbalance of two different types of such cells — pro-inflammatory vs. anti-inflammatory — are significantly higher among patients with rheumatoid arthritis than those without.
Among arthritic patients, the ratio of anti-inflammatory macrophages are lower than pro-inflammatory ones. This imbalance causes the rate of bone degradation to be much higher than the rate of bone formation.
Fulminant stage: The final stage is where you can no longer move your joints much or at all. As the term “fulminant” implies, the joints have fused together and rheumatoid arthritis is at full onset. There’s heavy damage to the cartilage and bone.
Also at this stage, there’s an increased risk of getting cardiovascular disease due to systemic inflammation.
Other complications include increased risks of :
- Reduced cognitive function
- Fatigue
- Lung tissue inflammation
- Fibrotic disease
- Sarcopenia
- Sjogren’s syndrome
- Cancer
It can take many years to reach the final stage, and everyone experiences different symptoms and speed of the progression.
Who is more likely to get rheumatoid arthritis?
About 0.5% of the world’s population suffer from rheumatoid arthritis, with people who live in urban areas have higher prevalence of the disease than those in rural areas.
In addition to genetics, certain viral infections, air pollutants, and obesity mentioned earlier, other factors that increase the likelihood of getting RA include:
Gender: Women are about three to four times more likely than men to get RA, but data suggests that it mostly pertains to women age 50 and under. At around age 60 for both genders, the ratio for women and men decreases to 2:1.
One reason why women are more likely to develop rheumatoid arthritis is because of higher levels of a certain form of estrogen hormone.
Age: While rheumatoid arthritis is often assumed to occur in older people, it can happen at any age.
Ethnicity: A 2017 review of nearly 8,800 Americans found that being full or partial Hispanic have lower risk of getting rheumatoid arthritis. The authors wrote that it could be a statistical issue since the majority of the sample (40.7%) are whites while the remaining samples are nearly 20% are Blacks (non-Hispanic), Mexican American and other Hispanics, and other ethnicities.
Socioeconomics: The same review also found that “living in poverty and covered by health insurance were also positively associated with rheumatoid arthritis,” but there is no cause-and-effect relationship established.
Other factors that can increase the risk of getting rheumatoid arthritis include having diabetes or osteoarthritis.
Getting enough sleep regularly and a lack of sufficient vitamin A intake were associated with a lower risk of rheumatoid arthritis. Again, the researchers only found associations, not causation.
Treatments
First, clinicians often use treatments that slow down the rheumatoid arthritis progression to the point where such progression is almost stopped and to prevent remission. In 2010, a task force of rheumatologists, other clinicians, and patients recommended such “treat-to-target” approach.
The task force was also updated in 2014, providing a more inclusive and holistic approach to patient care. This includes elements of narrative medicine, such as treating rheumatoid arthritis “based on a shared decision between patient and rheumatologist,” and the physician “should involve the patient in setting the treatment target and the strategy to reach this target.”
Medications
DMARDS (disease-modifying antirheumatic drugs) is one of the most commonly prescribed medications because of its success rate. They target specific molecules or pathways that are involved in rheumatoid arthritis inflammations.
“DMARDS are able to work on some of these pathways of inflammation to successfully change what’s going on in your body so [the immune cells] don’t attack you as much,” said Dr. Alexis Mobley, who earned her doctorate in neuroimmunology from The University of Texas. Mobley also suffers from rheumatoid arthritis since 2011.
“I think the one that surprised me the most is Methotrexate because that’s the first one that I was put on, and I had ever known it as a cancer drug,” she said. “I was like, ‘What? Are y’all putting me on chemotherapy? How could you?’”
Mobley said that there are different doses of methotrexate between cancer and rheumatoid arthritis patients, and the drug has been studied for many years with the latter group.
Other DMARDs that may be prescribed include sulfasalazine, leflunomide, and hydroxychloroquine. However, a 2019 systematic review found that “there was no consistent pattern in these recommendations” on a global scale.
The authors also mentioned that these global guidelines about DMARDs are pretty consistent worldwide. These include:
- Usage of combinations of conventional DMARDs
- Bringing different experts to collaborate on the usage of DMARDs in research and clinical practice
- Rheumatoid arthritis outcomes in the last two decades have “improved significantly.” This is likely because of how guidelines have improved the quality of clinical practice.
The guidelines aren’t set in stone, and they will be updated — as they often have been — as research and clinical care progress.
“Knowing that there are non-classical pathways of getting and treating inflammation is how I understand these DMARDs work,” Mobley said.
Mobley said that the future of treatments is targeting specific immune cells or proteins that cause rheumatoid arthritis and other connective tissue diseases rather than suppressing your entire immune system, like with DMARDS.
“Your immune system will still be mostly intact. You don’t have to be afraid of catching a cold or doing things that drastically change your lifestyle,” she said.
Occupational therapy and physical therapy
Like physical therapy, occupational therapy research also finds benefits of physical activity as an effective treatment. Educational and psychological approaches, such as cognitive behavioral therapy (CBT), are also effective in managing pain, function, depression, and independence.
A combination of aerobic, strength, and meditative exercises should be used for some patients. Occupational and physical therapists should collaborate with patients to find out which types of exercises would work best for each patient.
Living with rheumatoid arthritis

“It’s about riding the ebbs and flows, getting in when you can, sitting out when you can’t.” You gotta be unapologetic about it.” Photo: Alexis S. Mobley
While there appears to be no strong evidence between having rheumatoid arthritis and increased risk of getting COVID-19, many people connective tissue diseases are not taking any chances with the possibility of getting infected with another disease.
Mobley added there are psychosocial problems rheumatoid arthritis patients face during the pandemic, including depression, loneliness, and anxiety.
When the second wave of COVID-19 was coming down in the spring of 2021, Mobley felt more comfortable going out while still taking precautions.
“I was double-masking and going out at odd times when there aren’t many people to pick up some things,” Mobley said.
But with the rising number of cases and deaths in the U.S. due to the Delta variant of COVID-19, Mobley had to discontinue working in the lab at the university and stay home based on her doctor’s orders.
“I kept getting sick, I kept catching colds just from one to two hours of interactions at my job,” she said. “I know I’m not the only one that are put in similar positions of continuing to quarantine at home. There are a lot of people who never really got to leave, so some people who are upset [said] that, ‘Well, I got my freedom back,’ but there are millions of people who never got it in the first place and are still doing 18 months at home just trying to stay alive.”
Despite being stuck at home, Mobley is still able to do research by having her lab assistant, who is a graduate student, do the actual lab work while she analyzes and interprets the raw data that her assistant sends her.
Coping with rheumatoid arthritis and retaining independence
Mobley suggests that rheumatoid arthritis patients should find a community to join. For her, it was going back on Twitter and looking for people to reach out to.
“Find people, find community, find ways to reach out,” she said. “I know it doesn’t sound exciting, but it’s been the best way for me.
“I’m currently on several Discord servers, and [connect] with several disabled individuals whom I can identify with. I’m on several Twitter group chats, and CreakJoints has their own little chats once a month, #CreakyChats, and I absolutely love [it].”
Other than chats, Mobley also finds watching a stand-up comedy before bed helps her cope and go to sleep.
For doing daily activities, like showering, dressing, and cooking, Mobley suggested that you should use any mobility aids that you can get your hands on.”
“I know it sounds easy like just go to the store and get a shower stool or walker, but there are several layers to that,” she said. “There are some things you can’t change. If I can bring my stove down so I can sit and cook, I absolutely would.”
Because Mobley couldn’t stand for a long time, she adapted by cooking a huge batch of food one day and put it in the freezer so that can reheat the food for the next meal.
“It’s about riding the ebbs and flows, getting in when you can, sitting out when you can’t,” she said. “You gotta be unapologetic about it.”
Mobley and Davidson are part of CreakyJoints, an advocacy and support group for those living with rheumatoid arthritis. Mobley said that engaging on CreakJoint’s chats (#CreakyChats) seem to be more helpful than going to her doctor because she sees their tweets on Twitter or chat discussions that are “relevant to how she feels at the moment.”
Davidson said that taking care of herself beyond her joint pain, like exercise, having a support group, and working with different healthcare professionals.
“Educating myself, participating in research, volunteering with different organizations, attending classes,” she said. “There are so many free classes, like from the Arthritis Society and Arthritis Foundation. I took all of them.”
She later started to write and advocate for arthritis patients, which allowed her to cope. People who share her pain experience started to listen more and started to offer help. They did not dismiss her pain as being all in her head.
“It was a badge of honour because I was expressing myself rather than hiding it,” Davidson said. “I’m stuck with this feeling and coffee ain’t gonna fix it.”
Alexis Mobley is also the director of Blackimmune.org, a non-profit that showcases Black immunologists’ contributions to science from around the world. The group also provides resources to Black students and professionals for jobs in immunology and related fields.
You can follow Eileen Davidson for her updates and mini-adventures on Instagram.
Original publication date: Sept. 10, 2021. Updated for 2025.
Nick Ng is the editor of Massage & Fitness Magazine and the managing editor for My Neighborhood News Network.
An alumni from San Diego State University with a bachelor’s in graphic communications, Nick also completed his massage therapy training at International Professional School of Bodywork in San Diego in 2014. In 2021, he earned an associate degree in journalism at Palomar College.
When he gets a chance, he enjoys weightlifting at the gym, salsa dancing, and exploring new areas in the Puget Sound area in Washington state.