As a massage therapist who works primarily with relatively healthy clients in a spa or house-call environment, I never thought massage therapy has a pretty big role in mental health care. I mean, when someone is suffering from PTSD, Kurt-Cobain level of depression, or high enough anxiety that makes them want to rip paper slowly in strips all day long, I would imagine they would seek help from a qualified psychologist, psychiatrist, or even a chaplain or rabbi.
But a massage therapist? Even the “registered” subspecies? I wouldn’t imagine. But how do massage therapists play a role in working with patients or clients with mental health issues?

Last week, I attended the Registered Massage Therapy Association of British Colombia’s (RMTBC) first mental health symposium: Mental Health and the Body at the same place where last year’s manual therapy conference took place. It was a sold-out crowd of 350-plus registered massage therapists (RMTs), including a few physios and other manual therapists who were camouflaged among the herd.
Like the San Diego Pain Summit, I was impressed with the enthusiasm from most therapists as well as the quality of the presenters:
* Pam Fitch, RMT: Using Massage Therapy for Anxiety, Depression, and Insomnia
* Dr. Christopher Moyer, PhD: Massage, Anxiety, and the Autonomic Nervous System
* Dr. Robert Ley, PhD: Art & Science of Linking Talking and Touch Therapises in Treating Trauma
* Damian John, BA, RMT: Working With First Nations, PTSD, and Mental Health
* Dr. Cynthia Price, PhD: Massage for Disconnected Individuals Due to Stress, Pain, & Trauma
* Dr. Theresa Newlove, PhD + Dr. Amrit Dhariwal, PhD: Somatization and the Mind-Body Connection, Pathway to Collaborative Care
* Dr. Gabor Maté, PhD: Biopsychosocial View of Mental and Physical Illness
Several RMTs and organizers of the event were eager to share their knowledge and experience with Massage & Fitness Magazine.
M&F: Why is understanding mental health important for RMTs?
Bodhi Haraldsson, RMT, Director of Research of RMTBC: There is a need for all health care professions to respond to government (local, provincial, and federal) call for improved mental health care. At the same time, the field of massage therapy is seeing increased understanding on how touch- based therapies influence various psychological conditions. We are also seeing the psychosocial piece of a patient’s recovery from illness and injury is becoming better understood. For massage therapy to be further accepted in health care, we must understand the psychosocial components of care.
Lizette Tucker, RMT, Co- Chair , PPG Mental Health and Massage Therapy: It is important that RMTs have a general understanding of these conditions just like other pathologies. Although we may have an understanding of these conditions, our scope of practice prohibits us from counselling or providing any treatment outside of massage or manual therapy. We do not treat the condition, we treat individuals with those conditions. Having a sound understanding regarding mental health issues increases our ability to treat these patients effectively within our scope. Our scope of practice allows for us to develop a treatment plan that may include remedial/home care exercises.
As health care professionals that deal with many types of issues that may include everything from physical trauma due to a motor vehicle accident, or a work place accident, athletes, post surgical, to emotional trauma of cancer patients. To create a proper treatment plan for our patients, having this understanding will assist us in providing the best care possible to our patient, — within our scope of practice.
M&F: What changes do you think this conference would influence how massage therapists work with patients with mental health problems?
Haraldsson: This symposium was held to explore the issues and questions around the integration of mental health into our practices. It was a good opportunity for us to learn together, to foster cooperation, to interchange ideas, and build capacity to get ready for any upcoming challenges. I am confident that attendees brought home new ideas at the end of the day that helped enhance the overall practice of massage therapy. Our goal was to build the scientific bridges between mental health and the health of the body.
Tucker: This conference helped us recognize the types of patients we see and how we can best provide treatment. It also provided us with the results of research regarding what really happens with the body when an individual is depressed or even suffers from anxiety during a treatment.
I hope that over time we may be able to develop more thorough assessments of our patients that may include mental health questions if appropriate or at the least build an awareness for RMTs as to how stressed a patient is upon coming for treatment.
I also hope that RMTs will begin to collaborate with other healthcare professionals and the patient’s physicians regarding issues they feel may need to be addressed to increase better patient outcomes.
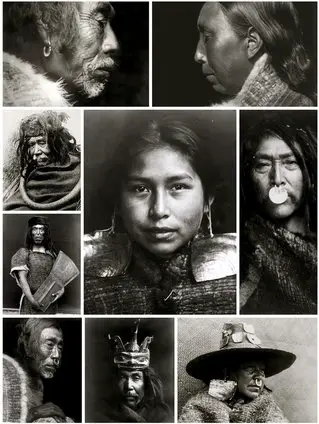
Personally, one of my interests is Damian John’s presentation on PTSD and the First Nations and what these topics have to do with massage therapy.
“I investigated and quickly realized that I know individuals who struggle or have struggled from PTSD related symptoms,” John explained to me in an email interview. “What I also realized is that the trauma as it relates to First Nations is much more complex than a single diagnosis, and as such, is a different beast to tackle, even in talking about the subject.
“So I broadened the conversation to include the idea of complex trauma, and this is where things get interesting because small, tribal, indigenous communities and their medicines as they relate to mental health, are very different than mainstream.
“From a massage therapy perspective then, is there a way in which we can make room for culturally specific health and wellness practices, both from the patients’ perspective as well as the therapists’ perspective? Is there a responsibility there for us as a health profession to account for these healing methods? Do they fit into our scope of practice? If not, should we be considering a more culturally sensitive scope?
“All questions that I think need thoughtful dialogue and due process.”

Some of the attendees gave their thoughts about what they had learned and digested.
M&F: Has this event change or influence the way you think about what and how you work in your practice?
Bruce Martell, RMT: Well, it’s hard to say whether this event will change the way I practice over the long term, but it’s easy to be enthusiastic about the information right now in the days following the symposium.
One thing I’m more conscious of since Christopher Moyer’s presentation is how I handle the neck and head. In his study, he monitored people’s arousal rates during the course of massage. Towards the end of the treatment, when the neck and head are being treated, these rates went up. He theorized this was because these areas are vulnerable and our nervous system may go into protection mode when we are being touched here. So I might be a little more gentle and make sure I do everything possible to make people feel safe when I’m treating the neck and head.
If anything, this event just reinforced my current mindset: that massage therapy is about how we connect with people. It’s not about pushing and poking muscles hoping to make a some sort of physical change. When we touch people, we are interacting with their nervous system, and their minds. The symposium brought this concept home for me.
Jannie Chow, RMT: I had a patient a long time ago who is incredibly high maintenance. [Some patients] usually have a lot of drama in their lives. I don’t know much about parenting, but their relationship with their parents affects their dependence.
I’m more compassion about it rather than being dismissive. At least I know where they’re coming from. Is it mine to do to “drain myself” to make them feel better? Not really, but I least I know how to set boundaries and not having the healer syndrome.
Ken G. Leong, RMT: It’ll take a while to remember, digest, and integrate everything that was covered in the conference, but it was a big reminder about how trauma is formed in the nervous system, not the other tissues, and how events can reverberate throughout the years, decades, and even generations in individuals and those connected to them. And it has deepened my knowledge and commitment to having a good biopsychosocial understanding of conditions and people whenever possible.
Ann Sleeper, RMT: Like many of us, I have spent my career paying attention to biomechanical causes of pain. Now that the biopsychosocial model is bringing psychological and social factors into the limelight, it’s an ongoing challenge to pull my mind out of the familiar channels of a purely structural viewpoint into the open waters of a more expansive world view. Like most manual therapists, I have always understood that a patient’s psychology, their life experiences, their work and family life and the society they live in are important. However, most of us have limited training in the specifics of how those things impact our patients other than a general understanding that they do.
In the past, I have seen my role as providing a kind and accepting ear to whatever my patients choose to tell me about their lives while I attend to my real business of working with the purely physical state of their tissues and nervous system. This conference increased my understanding that any emotional state, depression, anxiety, insomnia or trauma they may have are linked to the pain they have come to me to address. All those things can cause patients (and us!) to disconnect from their bodies and decrease physical awareness and emotional awareness.
Both the patient and I may be unaware of that, even as it is happening under our noses.
Now I more clearly realize that every time I touch a patient I am teaching them to pay attention to their bodies. I’m teaching their body how to feel itself. By bringing a patient’s conscious attention to an area of the body, I can help them wake up to what they are feeling, emotionally and physically. That is an important step for many people, and can help them recognize and manage both physical and mental stress.
So if that’s a big part of what I’m doing, best I know it. Then I can tell my patient and they will know it too. Manual therapists mustn’t be counselors. We don’t have the training. But we can be gentle teachers of the art of paying attention. So I’m going to give that a try.

M&F: Who is your favorite speaker(s) and why?
Martell: It would be hard to pick someone other than Gabor. he was very easy to listen to. He has a calming presence and a soothing voice, a personality that you instantly feel comfortable with, someone you could tell your deepest secrets to. And that’s just what happened during question and answer period as Gabor asked probing questions to some of the attendees. He spoke slowly and deliberately, and I had the feeling he was always on the verge of saying something truly remarkable, so i was hanging on every word.
As good as he was, Christopher Moyer’s presentation may have been my favourite. His research on patients’ autonomic arousal rates while receiving massage was fascinating. Take-home nugget: anxious people actually had higher arousal rates when receiving massage than if they just lay down without massage. Yet they still reported feeling less anxious after the treatment. I guess physiological measures don’t tell the whole story.
Anita Wilson, RMT: I found two of the speakers more influential for me, and maybe not for the obvious reasons. I suspect that others found interest in the speakers who addressed things from a clinician’s perspective, and/or who spoke of things that were obviously relevant to our scope of practice. I actually found my two favourite speakers were the ones who spoke more about the actual psychology and how it affects the individual, those being Dr. Gabor Mate and Dr. Robert Ley.
In speaking with a fellow colleague afterwards, it was interesting to me to hear that the very reason they may not have like these speakers as much was because they spoke of things outside our scope of practice. I maintain my strong opinion, however, that while treating the psychology (or actual trauma) itself is outside of our scope of practice, being “trauma-informed” is vital in upholding our practice standards and the safety for patients.
I found that Dr. Robert Ley focused mostly on trauma in our general population and drove home the reminder of how prevalent it is in our every-day patients (first responders, domestic abuse victims, children, etc). I feel that he helped identify the limits of cognitive (e.g. talk) therapy and emphasized the importance of somatic (e.g. touch) therapies in the resolution of symptoms for patients suffering from PTSD and other trauma.
I also found Dr. Gabor Mate’s presentation to be essential in challenging us to question the current definition of our Scope of Practice, and more importantly the interpretation of such by our own regulatory College. I find it absurd that our College uses, what I feel are, scare-tactics when discussing treatment of patients suffering from trauma and trauma-symptoms. How are we to effectively and, more importantly, safely provide treatment to our patients if we don’t understand what is possibly behind their presenting symptoms or condition?
It’s like asking a therapist to provide care (possibly for stress-management, muscle tension, headaches) for a patient suffering from cancer and telling them they cannot and should not ask anything about their cancer or other cancer treatment. How are we possibly able to use educated judgement on what to say, to do (or not say, not do), body position and body language, when to seek information from other attending care givers, when to refer back to those care givers, and most importantly whereas those boundaries in our scope of practice. If one is not informed, then how does one possible have intelligence in these matters. Common sense does not always prevail.
As mentioned above, I believe our college fails to adequately address and to clarify the vital difference in “treating trauma” vs. being “trauma-informed” in developing our treatment plans within our scope of practice.
Leong: It was primarily Dr. Gabor Mate whose presence drew me in. I have always aspired to be like and looked up to professionals who can quickly size up a situation — and give answers to the patient, and draw conclusions in really short order. Dr. Mate certainly did that, with his quick demonstration of questioning a few people who believed they had a happy trauma-free childhood, and demonstrating that things probably weren’t as pain-free as the people had thought.
Damian John, whom I wasn’t sure of being of interest to me initially, and even made me a bit skeptical and impatient with his introductory group breathing and meet and greet your conference neighbour session. Eventually he won me over with his generosity and courage in sharing the horrors that happened to his people and family in the deliberate and coldly executed destruction of his people’s culture, language, and family structure. He also made a cogent point in his portrayal of these factors, the lifestyle and culture being biopsychosocial medicine in of themselves. A tragic story to be sure, and also a warning to those of us in the present and future that these factors can heal or harm us as well.
Sleeper: Choosing my favourite speaker at the conference would be like choosing my favourite ingredient in a cake. It’s the overall mix that counts. Each of the speakers said similar things, each in their own way, about the inseparability of the mind and body and their impact on each other.
I did appreciate that Pam Fitch, RMT and Dr. Cynthia Price had experience in using touch to communicate with patients’ emotional/physical state and had some advice on how to go about it. Learning that it can be done is one thing. Knowing exactly how to do it is a different matter.
M&F: If RMTBC hosts another such conference again, what would you like to learn or addressed?
Chow: Can we bring Chris Moyer back? I want to learn more about his recent research regarding the prone and supine positions’ effect on relaxation and restfulness.
Wilson: I would love to see the next conference on Massage Therapy for Sport. I think this is a huge topic in the world of manual therapy and has possibly the widest spread population of both patients and therapists. Whether it be the armchair athlete, weekend warrior, amateur community competitor, or elite athlete, I would bet that every therapist has encountered someone in this demographic at some point in their practicing career. There is so much research available with regards to therapy in sport (both passive and active rehab, use of heat/cold, etc). The other interesting discussion that could or should happen is the discussion of RMTs or manual therapists as part of the IST (Integrated Support Team) in sport — discussions about the importance of RMTs as part of that team and the challenges of being asked to the table so-to-speak and in what capacity.
Sleeper: I would like more information on how to talk to patients about how their physical symptoms and emotional states might be intertwined. This can be new and even difficult information for patients and takes some training and skill to communicate well. It can be misinterpreted as “it’s all in your head” and if a patient hears that, they will not want to hear anything more.
There could be workshops after the conference so that speakers could teach participants more about working with patients in this way.
I would also like more information about where the line is between educating patients and becoming their counselors. The first is appropriate, the second is not. Those of us who have government licensure have regulatory bodies who are correctly concerned that we stay within our scope of practice. Other professions will be concerned with that as well. Most importantly, we must not do harm to our patients by going beyond the limits of our training.
Leong: Although mental health wasn’t necessarily on my dream list of conferences to attend, it was the speakers that drew me in, and now I see that without being aware of trauma, anxiety, and mental health issues, my practice is incomplete. And the knowledge gained just solidifies a holistic biopsychosocial understanding of the human and their whole journey. So I don’t necessarily have a personal agenda and look forward to being surprised by whatever is chosen in the future!
M&F: Will there be another conference like this in the future?
Haraldsson: This symposium is the latest in a series of cutting edge evidence based conferences hosted by RMTBC. In 1999, we held the world’s first massage therapy research conference. Since then we have hosted four evidence-based conferences. These conferences are an extension of the RMTBC vision for greater scientific understanding and utilization in the profession. It is our intention to continue on this same path. Next year, we are hosting a conference that focuses on all of our Professional Practice Groups (PPG). The newly established Mental health PPG will be represented there.
Tucker: We had a great response to the Mental Health and the Body Symposium. It sold out in matter of weeks, faster than other conferences that has been held by the Registered Massage Therapists’ Association of BC!
The speed at which RMTs and other health care practitioners registered supports my belief that there is a strong interest for this type of information. Unfortunately, until this symposium there have been limited professional development courses regarding mental health and the effectiveness of massage therapy, so this is a great starting point for the profession.
I’d like to say yes, but in the interim we hope that this event will drive the development of courses that educate RMTs on mental health and how massage therapy can be an integral component in the overall treatment of a patient. Given this, one of our first projects as the PPG Mental Health will be to research a Mental Health First Aid course for massage therapists.
Dr. Christopher Moyer: The integration of massage therapy science and practice is more impressive in British Columbia than anywhere else I have seen, and their conferences and events are the best. I wish it was possible for me to have a career pursuing this work so that I could keep attending their events. The events put on by the RMTBC are first rate, and I love interacting with the members who are so well-informed, professional, and engaged.
We would LOVE to hear your thoughts and feedback in the comments sections below about the event if you had attended. For those who could not go, share with us your thoughts about this event and other cool stuff RMTBC is doing.

A native of San Diego for nearly 40 years, Nick Ng is an editor of Massage & Fitness Magazine, an online publication for manual therapists and the public who want to explore the science behind touch, pain, and exercise, and how to apply that in their hands-on practice or daily lives.
An alumni from San Diego State University with a B.A. in Graphic Communications, Nick also completed his massage therapy training at International Professional School of Bodywork in San Diego in 2014.
When he is not writing or reading, you would likely find him weightlifting at the gym, salsa dancing, or exploring new areas to walk and eat around Southern California.





