Many massage therapists and personal trainers believe that they can stretch fascia or break adhesions with manual therapy, foam rollers, or other tools and methods. However, no quality evidence exists to date that says we can stretch or change the shape of fascia in any lasting or meaningful manner. The idea is just implausible.
Although “The Effects of Manual Therapy on Connective Tissue” by Dr. A. Joseph Threlkeld was published in 1992, the information is still relevant. (1) If we talk about the effects of massage and manual therapy on fascia or other connective tissues, we should be familiar with this important paper on the tensile strength of collagen fibers, the primary component of fascia. You can open the document and reference it to the “figures” mentioned in the paper.
Breaking down the fascia paper in manual therapy
The introduction describes how manual therapy encompasses a broad range of techniques that are usually intended to treat both pain and joint dysfunction. Some techniques are meant to affect connective tissues and include stretching, compression, massage, fascial/tendon stretching, traction, and thrust techniques. (Thrust techniques generally fall outside of the scope of practice of massage therapists.) This paper focuses on the effects of connective tissues structures that impair range of motion through abnormal connective tissues shortness or diminished connective tissues mobility. Connective tissues may act in concert with the shapes of bones at the joints or other structures to limit range of motion.
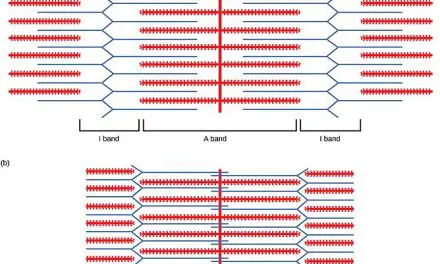
The next section on the mechanical behavior of connective tissues describes the structure of connective tissues. Note the similarity in structure of ligaments and tendons, whose collagen fibers are arranged in small bundles of mostly parallel fibers with a few fine elastic fibers joining them together. When not under tensile loading, such as stretching, the bundles may have small undulations or “crimping.” Fascial sheaths and aponeuroses also have collagen bundles but are organized into sheets and also may have undulations or waviness. Ground substance and elastic content is low in fasciae.
The waviness or crimping in the collagen fibers creates a variable amount of slack. This slack must be taken up before any individual bundle of collagen fibers is subject to stretch. Fibers directly parallel to the direction of stretch or those that have the least crimping will be the first to resist tensile loading. Collagen fibers generally will be aligned with the direction of force (movement) they resist. Fibers within a bundle will generally be parallel, but neighboring segments may not be aligned with each other so that the tissue can resist movement in various directions.
The resistance of a tissue to deformation — changing of its shape such as actually lengthening the tissue — can be illustrated on a graph as a stress-strain curve. The amount of stress placed on the tissue is plotted along the y-axis and the resulting deformation is plotted along the x-axis. Figure 4 of the paper shows an example of how a hypothetical stress-strain curve might work.
The actual stress-strain curve of any particular tissue in the body will vary. The beginning of the curve shows how in the beginning a small amount of stress on the tissue creates relatively great amount of change in the length as the slack is taken up in the wavy fibers and the fibers are pulled straight. This area at the beginning of the curve is called the toe region.
Figure 5 of the paper shows the stress-strain curve of a human anterior cruciate ligament (ACL). The beginning of the curve shows the normal amount of load and displacement (i.e. normal amount of movement) during an anterior drawer test, a common orthopedic test used to determine the integrity of the ACL.
The physiologic loading region is the region where the slack has been taken up and the collagen fibers begin to actually stretch. Within most of this zone, the fibers will stay intact. In daily activity, this represents the normal forces encountered by the fibers.
The fibers will stretch a little in response to being loaded but then return to their normal shape; they do not stay stretched. This non-permanent stretching is called “elastic deformation.” Just as an elastic band will return to its original shape once the tension on it is released, so the collagen fibers, when loaded within their tolerance, will return to their normal length when the forces on them are relieved.
Towards the end of the physiological loading region, at the highest levels of tension on the collagen fibers, one enters the region where micro-failure begins to occur. The shortest collagen fibers, if loaded beyond their tensile strength, will begin to break. Once these fibers start to break, the tissue will not be able to return to its original length and will be permanently lengthened.
There is a very small zone before micro-failure becomes injury. In other words, the breaking of small amounts of the shortest collagen fibers may result in increased range of motion, but the point at which this occurs very quickly turns into injury. Collagen fibers do not stretch in a manner that will stay permanent. The only permanent lengthening of the tissue occurs when the collagen fibers are broken.
Breaking of collagen fibers is a goal of some manual therapies practiced by physical therapists but may not be within the scope of practice of massage therapists. Breaking of collagen fibers is inevitably followed by inflammation, repair, and remodeling, which needs to be managed properly if the increased range of motion is to be maintained.
“The breaking of small amounts of the shortest collagen fibers may result in increased ROM, but the point at which this occurs very quickly turns into injury.”
Breaking fascia isn’t great, even if manual therapists can do so
Plastic deformation — the permanent elongation brought about by breaking collagen fibers — should not be confused with a phenomenon called “creep.” When a load is applied to a viscoelastic tissue over a prolonged period of time, the tissue will eventually assume a new resting length. This comes about through a redistribution of fluids in the tissues and is thought to be the mechanism by which some massage and manual stretching techniques may create temporary elongation.
However, once the stretching force is removed, the tissue will gradually resume its original length. Threlkeld suggests that research investigating manual therapy techniques should take measurements over an extended period of time in order to detect creep (and, presumably, not mistake it for a permanent improvement in range of motion). Maximum creep has been found to occur at six to eight hours. Creep deformation is not permanent and the tissue will gradually resume its original shape once the load is removed.
The elasticity of connective tissue can change depending on the rate at which loading is changed, a term called “coelasticity.” Connective tissue that is loaded quickly will behave more stiffly than tissue that is loaded more slowly. Figure 7 shows the difference between anterior cruciate ligaments that were loaded at a fast rate vs. a slower rate. The tensile strengths of various ligaments have been studied and it has been estimated that micro-failure of connective tissue begins at about three percent elongation and macro-failure at around eight percent.
Threlkeld states, “This gross approximation of the load necessary to cause microfailure (some permanent elongation) can be used to make some educated guesses about how effective the typical forces encountered in manual therapy will be in stretching connective tissues.” In other words, by knowing generally how much force it will take to cause collagen fibers to break, one can guess at how likely a manual therapy technique will be able to stretch connective tissue in any meaningful way.
The effects of injury and immobilization on connective tissues are described. When connective tissues are injured, the result is that the healed tissue has a more irregular arrangement, contains types of collagen fibers that are different than the normal fibers, has a lower water content, and has more cross-links between fibers, fiber bundles, and adjacent tissues (thus inhibiting sliding between bundles). The irregular arrangement of collagen fibers means that they are no longer aligned with the direction of force and will, therefore, have less strength.
Lower water content means the fiber bundles are less able to slide over and past each other. The end result of inflammation and immobilization is connective tissues that are less strong than normal tissue. [One could infer from this, then, that intentionally causing injury to connective tissue might cause more harm than good.]
Ethics behind ‘breaking’ fascia in massage therapy
Medical practitioners may use techniques intentionally meant to break collagen fibers to increase range of motion but these techniques (such as thrusting techniques) are clearly outside of the scope of practice of massage therapists. The amount, rate, and direction of force must be controlled within very narrow limits for it to be safe. Although these techniques are widely used, the forces actually applied during manual therapy are poorly documented.
No published estimates exist at all for the external forces developed during friction massage or soft tissue stretching. In light of what is known about the physical properties of the target connective tissues, there is no way to evaluate whether manual techniques can actually stretch connective tissues. Temporary lengthening achieved through soft tissue stretching could easily be misinterpreted as permanent lengthening.
Research supports the theoretical concept that force applied to connective tissues during remodeling after injury (that is, when the tissue is repairing itself and constructing new fibers) may improve the quality of the tissue, but it is unclear whether small doses of force (such as applied during manual therapy) would have any more effect than activity alone in actual practice.
External forces applied to the body are not directly applied to the target tissue and, therefore, not completely transmitted but are dispersed throughout the region, which will vary with the tissue and surrounding structures. The complex arrangements of fiber directions and other factors make real-world estimates of exactly how much externally applied force actually reaches the tissue difficult to measure.
Threlkeld concludes that physical forces can and do alter connective tissues. However, it would be easy to misinterpret this statement as supporting the idea that one can stretch connective tissues in a lasting manner without having read and understood the entire article. Forces generated by the body certainly effect the formation and organization of connective tissues and thrust techniques performed by medical practitioners most likely break collagen fibers.
Soft tissue manipulation by massage therapists, though, is not likely to generate forces that can permanently elongate connective tissue. This is the relevance of Threlkeld’s paper to massage therapists and other manual therapists.
(This article is was originally published in the Spring 2016 issues of Massage & Fitness Magazine. Edited Dec. 9, 2019.)
Reference
1. Threlkeld AJ. The effects of manual therapy on connective tissue. Physical Therapy, 1992 Dec;72(12):893-902.
Further Reading: Fascia Science Review
EXTRA!: A Word With Dr. A. Joseph Threlkeld
Although Dr. Threlkeld’s paper was published nearly 30 years ago, it is still considered relevant. The study revealed important information about connective tissue and so far the results have not been overturned by later research. Alice Sanvito contacted Dr. Threlkeld and asked if there were more recent research that either supported or contradicted his findings. Dr. Threlkeld attached a copy of a more recent paper by Chaudry et al. (1) published in 2008 and commented:
“I have attached another journal article that expands on my ’92 publication. These authors use mathematical modeling to predict connective tissue stress in three dimensions. They also collect some data from a treatment applied by a Rolfer. Their conclusions are similar to mine in that the forces generated in typical dense connective tissues by manual therapy treatments are much too low to produce permanent elongation.
“They also looked at the much less-organized tissue around the nose and estimated that manual forces might cause elongation in that tissue. I agree with their observation but would argue that the tissue around the nose is composed of various types of collagen, is loosely organized (to allow for mobility), and contains high proportions of elastic fibers and glycosaminoglycans. The para-nasal tissue is definitely not representative of most subcutaneous connective tissue nor would it be at all similar to scar tissue.”
“The three-dimensional model’s equations revealed that very large forces, outside the normal physiologic range, are required to produce even 1% compression and 1% shear in fascia lata and plantar fascia. Such large forces are not required to produce substantial compression and shear in superficial nasal fascia, however.” ~ Chaudry et al. (2008)
The Chaudry paper examined the effects of shear forces and compression forces on the plantar fascia, fascia lata, and nasal fascia of a live volunteer. Forces were applied by an experienced Rolfer trained at the Rolf Institute in Boulder, Colorado. The authors state in the beginning of their paper:
“The question of whether the applied force and duration of a given manual technique (eg, myofascial) could be sufficient to induce palpable viscoelastic changes in human fasciae is unresolved, with some authors supporting the likelihood of such an effect and others arguing against it.”
Their conclusion?
“The palpable sensations of tissue release that are often reported by osteopathic physicians and other manual therapists cannot be due to deformations produced in the firm tissues of plantar fascia and fascia lata. However, palpable tissue release could result from deformation in softer tissues, such as superficial nasal fascia.”
In other words, we cannot deform or stretch fascia in a way that it will remain elongated with manual therapy.
1. Chaudhry H, Schleip R, Ji Z, Bukiet B, Maney M, Findley T. Three-dimensional mathematical model for deformation of human fasciae in manual therapy. J Am Osteopath Assoc. 2008 Aug;108(8):379-90.

Alice Sanvito, LMT
Alice is a massage therapist who maintains a private practice in St. Louis, MO, She has been committed to client-centered, science-compatible massage therapy since 1991. She assisted at NMT seminars for the NMT Center of St. Petersburg, Florida, for 10 years and studied Russian Medical and Sports Massage with the late Zhenya Kurashova Wine for over 10 years, under whose direction she taught Russian Massage for three years.
Most recently she has studied DNM under physiotherapist Diane Jacobs. Alice has a particular interest in pain rehabilitation and enjoys working with performing artists, athletes, and pregnant women. When not devoted to her practice, you can find her playing old time music and dancing every chance she gets.