The letters that follow your name (like “LMT,” “CMT”) identify your responsibilities and limitations. Your title defines the who, what, when, where, and how of your professional scope of practice. Confusion, frustration, and resentment shadow many massage professionals’ understanding of their place among other wellness providers.
“Are certain modalities exclusive to my profession?”
“How much overlap exists between similar professions?”
“What happens if I break the rules?”
As any attorney will tell you, the answer to each of these questions is: “It depends.” Your practice act, if you have one, is the best place to find clarity (or, at least to begin searching for clarity). As one court observed, “[f]ew areas of governmental activity affect the public as much as the regulation of healthcare.” It went on to explain that legislatures and regulatory bodies are the ideal rule-makers in this area, and that our “complex and sensitive” healthcare system is best served when these issues are not hashed out in court.” When courts decide to ‘stay out’ of an issue, it can leave ambiguity until legislators or regulators provide guidance.
Providers might be frustrated by the lack of bright-line rules, but the murkiness surrounding scope of practice questions simply reflects the complexity of humans. Thus, the best way to approach scope of practice is with eyes wide open.
Be inquisitive, work collaboratively with neighboring professions to improve your understanding, and ensure that your treatment decisions reflect your patient’s needs. It’s rare that a single profession has all the answers to a client’s dysfunction and can, alone, solve the client’s ailments. Rather than viewing scope of practice as a restriction, try casting it as an opportunity for collaboration, creativity, and education.
What is the scope of practice of massage therapy in the U.S.?
The American Massage Therapy Association explains that scope of practice includes the “approaches you are specifically trained and competent to practice,” the “‘what’ and ‘when’ of health conditions you can work with,” and “your legal credentials/licenses.” It also considers your focus, practice environment, and working relationships with other health professionals. (2)
To many’s surprise, scope of practice focuses more on skills than legal credentials. When you offer services that are not aligned with your focus, practice environment, or skills, your treatments fall outside of your competency (in the eyes of the law). If you offer the treatment anyway and get sued, a court could determine that you were negligent in administering care.
Scope of practice questions often showcase a tension between clarity and flexibility. Massage therapists’ scope of practice is enshrined in their practice act, offering the benefit of clarity. Personal trainers, however, typically are not licensed by the state, and they arguably enjoy the benefit of flexibility in that freedom from regulation. Personal trainers (and other professions too) have veered away from licensure and have effectively taken a “free market” approach. That is, they educate and certify from within, and for the most part, only those who are ‘brought up’ through the profession will succeed professionally.
Neither state licensure or a “free market” approach is perfect. State licensing boards frequently demand that non-licensed massage therapists cease their operation of massage practices; and, plenty of incompetent and untrained personal trainers enjoy fruitful careers.
To many’s surprise, scope of practice focuses more on skills than legal credentials. When you offer services that are not aligned with your focus, practice environment, or skills, your treatments fall outside of your competency (in the eyes of the law). If you offer the treatment anyway and get sued, a court could determine that you were negligent in administering care.
State licensed professions may become fearful of “losing out,” and they aggressively lobby to define their scope of practice in state law. For example, acupuncturists have successfully staked a claim to the exclusive use of acupuncture needles — a move that has been fought by the physical therapists whom this deprives of offering dry needling treatments. These fights sometimes devolve into disputes over the nitty-gritty details of practice and create even more ambiguity.
This is particularly true among professions that are less protective of “their” modalities and client populations and more welcoming of multidisciplinary collaboration. For example: In Illinois, the acupuncture practice act states that acupuncture involves the use of needles, and the physical therapy practice act omits mention of needles. And the near-unanimous consensus is that physical therapists cannot use needles.
From my perspective as an attorney, I would surmise that if the legislature intended to allow physical therapists to use needles, they would’ve said so when writing the law. Intuitive? Far from it.
In Illinois, both the practice of physical therapy and massage therapy are defined by their respective practice acts. The purpose of massage is to “enhance the general health and well-being of the mind and body,” while physical therapy focuses upon the alleviation of impairments, functional limitations, or disabilities.
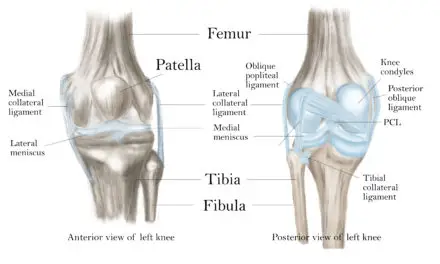
Though the physical therapy act does not mention diagnoses, massage therapists are explicitly prohibited from diagnosing. While the massage therapy act focuses on “structured palpation or movement of the soft tissue of the body,” the physical therapy act focuses broadly on therapeutic and rehabilitative massage and exercise. Essentially, the two acts alternate between clarity and vagueness, such that it’s not clear which modalities fall under which professional’s umbrella.
Scope of practice can dance a fine line between helping and hurting
Imagine you’re a pain patient who knows nothing about these professions. Would you know whether to visit a physical therapist or massage therapist? While most massage therapists are trained in multiple modalities, none are trained in all modalities. When your patient’s needs fall outside of your competency, treatment necessarily falls outside of your scope of practice.
For example: You’re a massage therapist who specializes in pediatric massage for people with sensory disorders. One of your longtime patients is no longer a child, but you’ve been treating her for 10 years and you’re confident that your specialization in her condition, extensive continuing education in the field, and collaboration with other professionals equips you to competently continue treating her. Today, she tells you that she’s pregnant.
You’re not trained in or offer prenatal massage, nor do you work with anyone who treats prenatal clients. You feel uncomfortable treating her while she’s pregnant but equally uncomfortable turning her away. What is and isn’t within your scope of practice ?
Continuing to treat her as if nothing has changed likely violates your scope of practice – and it puts her at risk. Instead, try collaborating with a prenatal massage therapist to offer integrated sessions with you both, or refer her to a prenatal massage therapist for the duration of her pregnancy. The solutions may not be easy or quick, but they should keep your patient’s safety as the focus.
This example highlights an often-overlooked nuance: just because your act permits a practice doesn’t mean that it within your scope of practice. Instead, your skills, experience, and practice environment should also instruct your practice. If you’re a massage therapist, your collaboration with and referrals to professionals like physical therapists and other massage therapists will enhance your professional integrity. By sticking to what you know, you protect your patients’ health, your reputation, and your ability to focus on your specialization.
Before asking if you can do it, be sure you want to do it
Rather than focusing on whether you can offer a particular treatment, take a step backward and ask if it’s a treatment that you want to offer. It’s human nature to suffer from Grass-is-Greener Syndrome. This focus on what’s just beyond our capabilities often overlooks the richness of those things that we can do with excellence and joy.
With a focus on your current treatment approach, ask yourself why you want to expand your modalities. Imagine that you are a physical therapist who currently utilizes 100 percent hands-on manual therapy with no assistive devices (like ultrasound machines) and no needles. You’re considering integrating dry needling into your practice, and you’ve asked me to offer my legal opinion as to whether it falls within your scope of practice .
I would ask why you want to offer dry needling. Is it a good business decision? Do you have clients who want to receive it? If so, do you credibly believe it will help them? And, if it is within your scope of practice, are you prepared to comply with the other requirements that such treatments will necessarily impose upon you?
For example, are you equipped to comply with state health regulations on the disposal of sharps? Does your building allow you to dispose of biohazard waste? Can you afford the costs of compliance with these and other regulations?
What does science say about a modality?
Another reason you might wish to avoid a particular modality is because it isn’t supported by science.
As an attorney with no medical training, this question always falls outside of my scope of practice. I encourage my clients to research the modality in current scientific journals and to talk with peers. Also, don’t cabin your research to your profession; sometimes another profession will have debunked or validated the effectiveness of a treatment.
Is your practice going to make your life more difficult?
Let’s say you’re considering expanding your therapeutic massage practice into the arena of medical massage, complete with insurance reimbursements. This may be an excellent way to grow your practice. It will also, however, subject you to a battery of government regulations. Are you prepared to meet the mandatory hurdles associated with being a medical provider?
You’ll need to hire an attorney to write your HIPAA privacy policies, purchase electronic medical records software, and get up-to-speed with billing codes. Private and governmental insurance systems present divergent requirements, and impose a hefty regulatory burden on participants. If you’re not prepared to meet these standards, then whether your scope of practice allows you to perform medical massages is irrelevant.
Carrots and sticks of scope of practice laws
Scope of practice laws are enforced by carrots and sticks — that is, by incentives and penalties. Regulators typically learn of scope of practice violations in one of two ways: (1) a regulator identified you as violating the law after posing as a patient, or (2) a patient or other professional filed a complaint against you.
If you’re investigated for violating your scope of practice, it will be very expensive. You’ll need to hire a defense attorney, and potential penalties include fines, loss of license, and criminal charges.
The well-being of individuals seeking your services is best served when you stay within their scope of practice. Representing yourself as a jack-of-all-trades does not serve your clients’ needs and does not inspire confidence in your abilities.
Your scope of practice compliance checklist
1. Familiarize yourself with your practice act and its regulations, and understand how they are enforced. Don’t worry about other professions; you’re only bound to comply with your own.
2. Know your ethical rules. Ethical rules are sometimes in your practice act or its regulations. Occasionally, your practice act will direct you to follow a national trade organization’s “model rules” instead. But be careful: unless your practice act says otherwise, the “model rules” aren’t dispositive as to your ethical obligations.
3. Create detailed written policies and procedures that govern your practice. Clarify what activities are within your scope of practice. Describe how you maintain your compliance with the various aspects of your practice act, ethical rules, and any other applicable regulations. Include the ways that you ensure ongoing compliance with your liability insurance policy, lease, business associate agreements, municipal zoning requirements, and business license.
4. Educate your patients or clients. Explain how your work jives with that of your patient’s other providers, and give your patient reasonable expectations for what they should and should not gain from your treatments. By setting expectations at the outset, you can clarify potential misunderstandings as to what services you can and cannot offer.
5. Be sure you have comprehensive professional liability insurance. Your insurance policy does not govern what is within your scope of practice, but it does articulate what claims are covered. Read your policy for specific exclusions. If your insurer doesn’t cover a modality, that doesn’t necessarily mean it’s outside of your scope of practice. Rather, it could mean that, in your insurer’s opinion, it’s too risky to be covered. Either way, ask: why does my insurer think the modality is risky?
On a personal note…
I healed from years of tortured chronic pelvic pain because a multidisciplinary team invested in and collaborated about me. It took a resourceful, compassionate, and humble team of a doctor, physical therapist, and massage therapist to give me the education, manual therapy, and medical support needed to facilitate a full recovery.
I’m grateful that those practitioners didn’t think that they could do everything, but instead recognized the limits of their skills, education, and licensure and enthusiastically collaborated with one another. They each broadened their familiarity with my condition, maintained firm compliance with the law, and most importantly, helped their patient: me.
Erin Jackon at the patient panel at the 2018 San Diego Pain Summit
Erin Jackson on Twitter: @healthy_lawyer. Email at ej@jacksoncompliance.com
(Feature photo: Ian Allenden/123rf.com)

Erin Jackson, MA, JD
Erin is a health and wellness attorney in the Chicago area at Jackson LLP. She also co-founded Jackson Compliance, a healthcare consulting company which specializes in practice start-up and compliance.
Through this work, Erin collaborates with providers to make their practices friendlier and more approachable for a diverse patient population. Erin strives to help her clients understand the provider-client relationship and become industry leaders in patient-centered care.