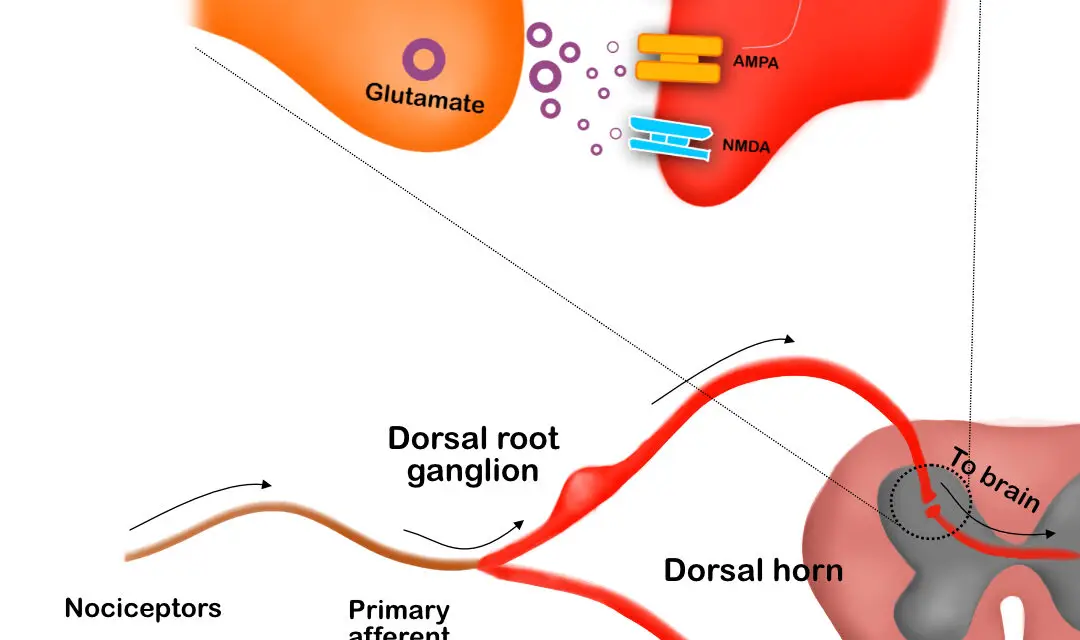
Central sensitization describes adaptations that occur in the brain and the spinal cord in response to repeated stimulation on your skin. The increased responsiveness comes in two main forms: hyperalgesia or allodynia. These changes are often part of the course of chronic pain, fibromyalgia, and chronic regional pain syndrome (CRPS).
Hyperalgesia means you feel even more pain than an already painful stimulus would create. If you have ever had a sunburn, you have likely experienced hyperalgesia when taking a hot shower after being in the sun. The sunburn was already painful but the increased sensitivity of the nervous system makes the heat from the hot water feel even hotter.
Allodynia refers to a situation where already excited nerves perceive pain when pain is not otherwise expected by that stimulus. It’s often reported as a symptom of CRPS (or reflex sympathetic dystrophy or RSD) where sufferers note that even their clothes touching their skin evokes pain. It’s also believed that this type of central sensitization plays a role in migraines as those who experience them often describe pain with brushing their hair or washing their face.
Comparison of the average sensation to nociception and light touch with hyperalgesia and allodynia. (Image by Nick Ng)
Peripheral vs. central sensitization
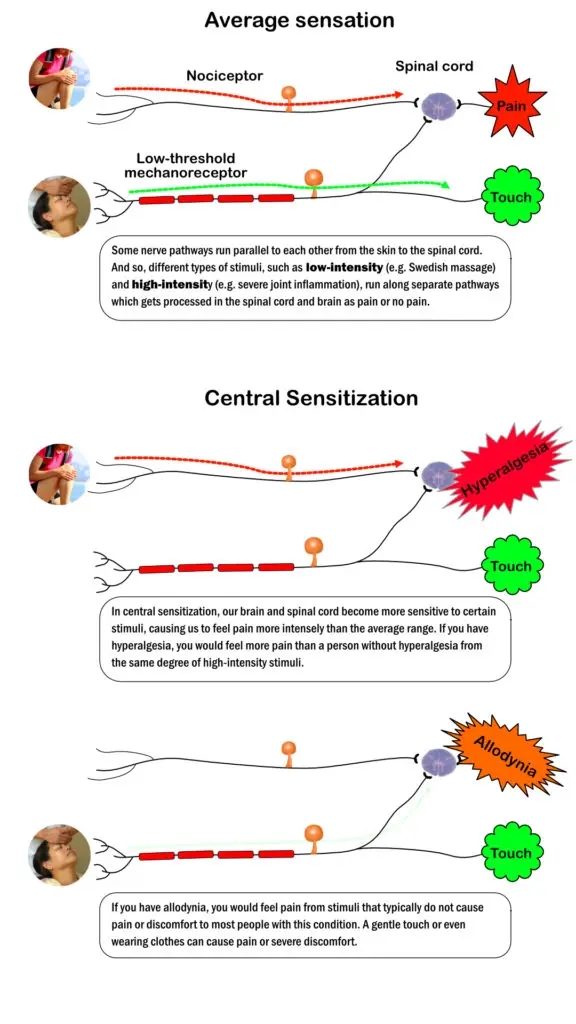
The peripheral nervous system is made up of the nerves that travel from the brain and spinal cord out to the rest of the body. When the afferent nerves—those that carry information to the brain and spinal cord for processing—are in a heightened state of nociception, it’s called peripheral sensitization.
On the other hand, central sensitization describes changes in nociception in the central nervous system. The main difference between the two types of sensitization seems to be that peripheral sensitization is heat-sensitive where central sensitization is sensitive to mechanical changes. Simply stated, someone with peripheral sensitization would experience increased pain with the heat application whereas someone with central sensitization would feel increased pain with a pin-prick. Both peripheral and central sensitization likely play a role in chronic pain.
Central sensitization and peripheral sensitization on the molecular level. (Image by Nick Ng; white blood cells by Blausen.)
What does central sensitization feel like?
A 2010 study in Manual Therapy surveyed expert clinicians to create a list of clinical criteria based on their consensus that could be used to diagnose different types of pain and to describe what central sensitization often feels like. They include:
- Local pain in an area of injury or dysfunction
- Local pain with palpation
- Painful postures or movements
- Absent or expected findings of hyperalgesia and/or allodynia
Central sensitization is characterized by:
- Disproportionate, non-mechanical, unpredictable pattern of pain in response to multiple, non-specific aggravating/easing factors
- Disproportionate, inconsistent, non-mechanical/non-anatomical pain in response to movement or mechanical testing
For example, if you are experiencing central sensitization, you may feel pain from something as simple as your shirt sleeve touching your arm or the wind blowing across your skin. You may also have pain that is far beyond what is expected from a minor injury, such as stubbing your toe.
Additional criteria that may aid in the diagnosis of central pain are:
- History of failed interventions
- Diffuse, non-anatomic pain and tenderness to palpation
Also, the experts agreed on these descriptors of peripheral neuropathic pain:
- Pain that was described as burning, shooting, sharp, aching or electric shock-like
- Pain or symptoms provoked with mechanical/movement tests that move, load, or compress neural tissue
Additional criteria that may be helpful in the diagnosis of peripheral neuropathic pain are:
- Pain referred in a dermatomal/cutaneous distribution
- Pain or symptom provocation with subjective aggravating/easing factors
- Clinical tests that move or stress neural tissue
- Pain or symptoms provoked by touch
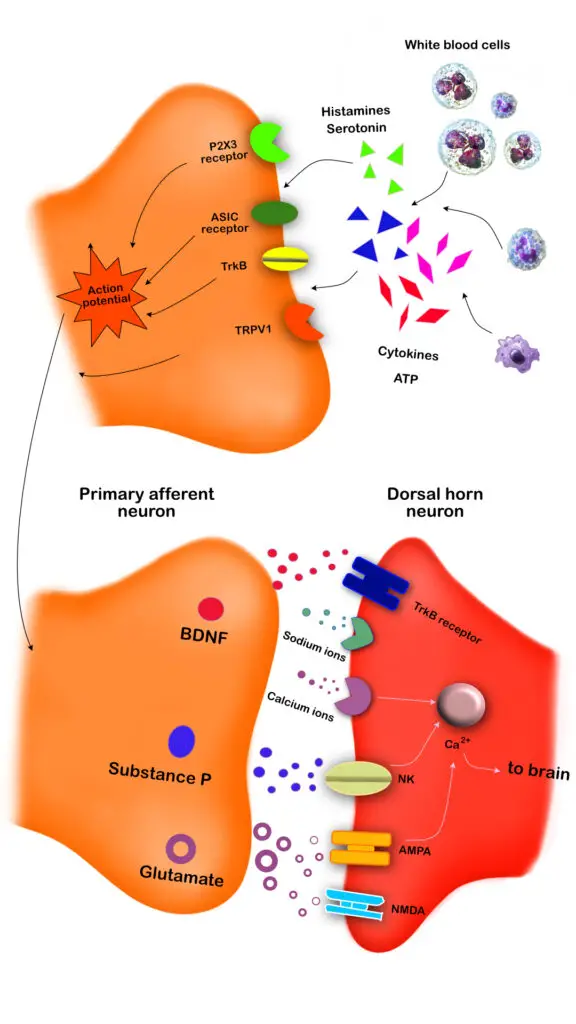
What causes central sensitization?
No one really knows what causes central sensitization, but research has shown that it is likely multifactorial. On a molecular level, there is too much activity at the junction between the neurons at the dorsal horn of the spinal cord and the peripheral nerve. This causes inflammation at the site, which lowers the pain threshold of the dorsal horn. Thus, this helps to explain why people with chronic pain experience allodynia and/or hyperalgesia
It’s widely believed that there are psychological and physiological components related to stress and anxiety. Studies have shown a relationship between stress and pain thresholds, meaning you experience more pain when your stress levels are elevated.
Also, those who experience pain-related anxiety consistently report higher pain levels. Taken together, these findings suggest that the state of the nervous system prior to the onset of pain can be a determining factor in the development of central sensitization.
Poor sleep quality and depression may also play a role in increased sensitivity to pain since there seems to be an inverse relationship between sleep the two, as well as pain (less sleep leads to more pain). The association between sleep and pain has widely been explored over the past two decades. Studies also suggest that insomnia may increase the risk of developing future chronic pain.
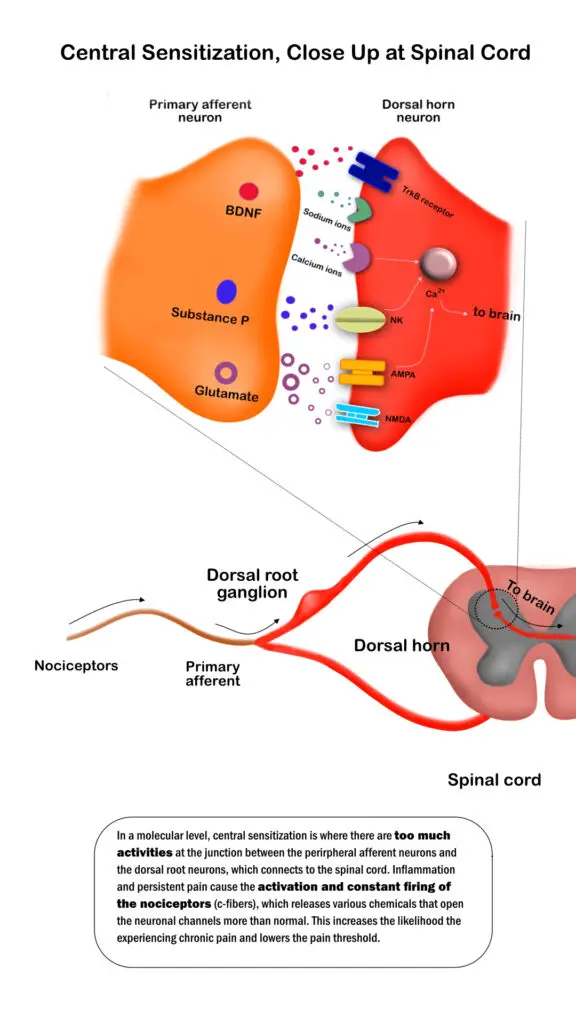
Central sensitization on the molecular level. (Image by Nick Ng)
How do you cure central sensitization?
There are several strategies that can help reverse central sensitization. Health care professionals may use pharmacological therapies, cognitive behavioral therapy, exercise, or even sleep therapy.
- Medications that could be included in a treatment plan may address inflammation, depression, and/or pain. Anti-depressants in particular are thought to address both the psychological component as well as treat physical pain; in the absence of depression symptoms, these medications may be prescribed at lower doses for purely pain management.
- Cognitive behavioral therapy (CBT) can help reverse central sensitization by providing you with strategies to change the negative thoughts or emotions that you associate with pain. CBT has also been useful in addressing depression and anxiety which can influence the development of central sensitization.
- Exercise therapy may include yoga, tai chi, strength training, flexibility training, aerobic exercise, or simply walking. Exercise has been shown to reduce pain, boost mood, and improve overall quality of life.
How massage therapy affects central sensitization?
There are several elements of central sensitization that may be helped by massage therapy. First and foremost, massage therapy can relieve pain. Even if only for a short period of time, in cases of central sensitization, any relief is welcomed.
Massage therapy can also decrease sensitivity through repeated touch. Called desensitization, this technique involves touching and stimulating the painful area to reduce hypersensitivity. It’s worth noting that this can take multiple visits to a massage therapist and may involve self-massage in order to get lasting effects, such as using a foam roller.
Massage can have multiple psychological benefits including improving mood, overall relaxation, and sleep quality. Using massage to manage stress levels, decrease feelings of anxiety, and improve sleep can address central sensitization while providing pain relief.
Related links
Video on central sensitization by PhysioTutors
Central sensitization explained by Dr. Andrea Furlan

Penny Goldberg, DPT, ATC
Penny Goldberg, DPT, ATC earned her doctorate in Physical Therapy from the University of Saint Augustine and completed a credentialed sports residency at the University of Florida. She is a Board Certified Clinical Specialist in Sports Physical Therapy.
Penny holds a B.S. in Kinesiology and a M.A. in Physical Education from San Diego State University. She has served as an Athletic Trainer at USD, CSUN, and Butler University.
She has presented on Kinesiophobia and differential diagnosis in complicated cases. Penny has published on returning to sports after ACL reconstruction and fear of movement and re-injury.
Outside of the clinic, Penny enjoys traveling, good cooking with great wine, concerts, working out and playing with her dogs.